In this issue of Blood, some of the controversies surrounding optimal therapy for patients with AIDS-related lymphoma (ARL) are now clarified by the analyses of Barta et al.1
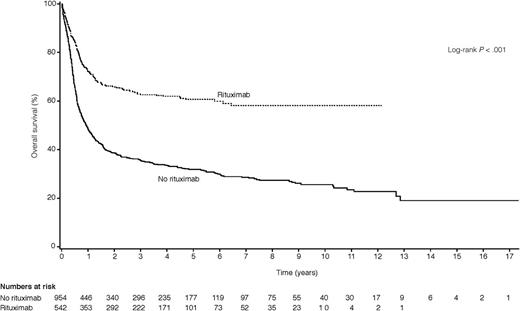
OS for ARL patients treated with rituximab-containing regimens vs those treated with regimens that did not contain rituximab. See Figure 2 in the article by Barta et al that begins on page 3251.
OS for ARL patients treated with rituximab-containing regimens vs those treated with regimens that did not contain rituximab. See Figure 2 in the article by Barta et al that begins on page 3251.
The profound immunodeficiency characteristic of HIV infection serves as an etiologic factor in the pathogenesis of ARL while also limiting the efficacy of standard multiagent chemotherapy due to development of intercurrent life-threatening infections, as well as depletion in bone marrow reserves. Prior to the availability of combination antiretroviral therapy (cART), use of standard multiagent chemotherapy was extremely difficult due to these factors, and low-dose chemotherapy was advocated.2 The introduction of cART provided a stunning reversal in prognosis, with an increase in overall survival (OS) among those with full-blown AIDS and a decrease in development of AIDS-defining conditions among those with HIV infection alone.3 Although concomitant use of cART and multiagent chemotherapy was shown to be safe in terms of pharmacokinetics,4 concerns remained about additive depletion of bone marrow reserve, potential overlapping toxicities, and limitations of chemotherapy dosing. At the same time, initiation of cART at the conclusion of systemic chemotherapy was shown to be an effective paradigm, as demonstrated by the initial infusional etoposide, prednisone, infusional vincristine, infusional doxorubicin, and cyclophosphamide (EPOCH) trials from the National Cancer Institute.5 Despite an increase in HIV viral load and a decrease in CD4 cells during the course of EPOCH, these parameters returned to baseline within 6 to 12 months following (re-)institution of cART. Although this study demonstrated that control of HIV viral load was not required for attainment of complete response (CR), still, development of opportunistic infection occurred in 8% of the initial EPOCH-treated patients within the first 3 months of completion of chemotherapy, and patients with CD4 cells <100/mm3 fared significantly worse than those with more intact immunity. Would these patients have done better if cART had been given earlier, concurrently with chemotherapy? A recent study from the AIDS Malignancy Consortium (AMC), in which patients received concomitant cART and chemotherapy, found that approximately half of complete responders had CD4 cells <100/mm3 at study entry, with a viral load >50 000 copies/mL, indicating that control of HIV infection is not mandatory for attainment of CR.6 The paper by Barta et al1 brings further clarity to this question by demonstrating that concurrent use of cART and chemotherapy was associated with statistically improved CR rates, with a trend toward improved OS among 1546 patients with ARL, studied as part of 19 prospective trials. Thus, although it is clearly possible to attain CR in the absence of concurrent cART, results are likely to be improved when cART is added. This is an important finding from the analyses of Barta et al.
Whether to use rituximab with chemotherapy has been another controversy in terms of ARL patients. Although clearly associated with improved outcome in patients without HIV infection,7 early studies from the AMC indicated that rituximab was associated with a statistically significant increase in infectious death,8 leading to the conundrum: to use or not to use? Careful evaluation of the AMC data, however, demonstrated that the infectious deaths occurred primarily among patients with CD4 counts <100/mm3. Further, subsequent studies from the AMC and elsewhere failed to confirm the initial conclusions, demonstrating that rituximab could be used safely with chemotherapy, without an increase in infections or death due to infection.6,9 As shown in the figure, the current analyses by Barta and colleagues has further confirmed the importance of rituximab in this setting, leading to a statistically higher CR rate, as well as improved progression-free survival and OS. Although these findings were limited to patients with CD4 cells >100/mm3 in the study of Barta et al, it will be important to next define the optimal regimen(s) for those with more profound immunodeficiency.
The Barta et al study has provided important data on large numbers of ARL patients, treated prospectively and evaluated using patient specific data. While serving to address several controversial areas, it is important to understand the limitations of this study. Although data were analyzed from 1546 patients enrolled in 19 published trials, a total of 23 such trials were excluded, and 1 included trial was taken from a letter to the editor and a second was from a published abstract. Only 2 of the included studies were phase 3 randomized trials, and approximately one-third of all included subjects came from one center.10 The exclusion of so many trials and patients may raise some question as to the validity of the conclusions. Additionally, many different regimens were used in patients treated over the course of 20 years. To analyze the data, the authors combined the various regimens into groups, as more or less intensive, infusional or not, and including rituximab or not. Again, this grouping may obscure the facts concerning use of one type of chemotherapy vs another. Despite the large numbers of patients, certain treatment groups were too small to draw conclusions, and although infusional regimens were found to be superior to those administered by bolus, this was only statistically confirmed when the infusional regimens under study were combined in the group as a whole. Further, the use of CR as an end point in the Barta et al analysis is made more difficult by the lack of uniform evaluation criteria for determination of CR, as well as lack of central review of these staging and restaging data, making verification of CR less than optimal. It is hoped that the ongoing phase 3 randomized trial comparing rituximab-cyclophosphamide, doxorubicin, vincristine, and prednisone with rituximab-EPOCH in HIV-negative patients with diffuse large B-cell lymphoma (CALBM50303; clinicaltrails.gov NCT00118209) will answer this question more carefully.
Will we ever have a fully “clean” data set from which to derive final treatment recommendations, based on level 1 evidence? Probably not, as HIV-infected patients, as well as the oncologists who treat them, tend to feel very strongly about use of concurrent chemotherapy with cART and/or use of rituximab. These inherent beliefs have confounded the ability to enroll patients on prospective, randomized trials. Given these realities, the paper by Barta and colleagues has provided helpful information, which may serve our patients well.
Conflict-of-interest disclosure: The author declares no competing financial interests.