Abstract
Viral infections lead to activation of coagulation which enhances inflammatory responses. For instance, influenza A is associated with activation of coagulation and the increased risk for thrombotic events, such as myocardial infarction. Protease-activated receptor 4 (PAR-4) is the main functional receptor on mouse platelets. Here, we investigated the role of tissue factor (TF) and platelets in influenza A infection in mice.
We used male LowTF mice, which express 1% of normal TF levels, PAR-4 deficient mice and respective control mice. All mice were infected intranasal with influenza A H1N1/PR8. Changes in body weights and survival were analyzed up to 14 days after infection. In addition, bronchoalveolar lavage (BAL) was collected and analyzed 7 days after virus challenge.
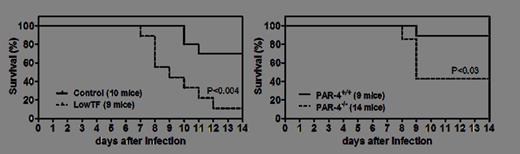
LowTF mice exhibited increased loss of body weights compared to littermate control mice between day 4 and 6 after infection (P<0.05). At day 7, BAL of LowTF had increased levels of free hemoglobin compared to infected control mice (2.60±0.39 g/dL vs. 0.05±0.02 g/dL, P<0.05). In addition, LowTF lungs exhibited increased protein levels in the BAL compared to controls (1.52±0.18 mg/mL vs. 0.70±0.26 mg/mL, P<0.05). Lung histology revealed that LowTF mice had extensive hemorrhages. The impaired hemostasis resulted in increased mortality in LowTF mice compared to control mice (90% vs 30%, P<0.004, N=9-10, Figure). Similarly, mice with defective thrombin signaling in platelets (PAR-4-/-) exhibited visible lung hemorrhages with increased hemoglobin levels in the BAL (P<0.05) at day 7 and increased mortality compared to controls (57% vs 10%, P<0.03, N=9-14, Figure).
TF mediated activation of coagulation and PAR-4 dependent platelet activation are essential for pulmonary hemostasis during influenza A infection.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.