Abstract
We analyzed hospital-wide red blood cell (RBC) utilization and indicators for clinical patient outcomes at Stanford Hospital and Clinics (SHC) after implementation of real-time clinical decision support (CDS) for RBC transfusions consisting of a best practice alert (BPA) within the computerized provider order entry (CPOE).
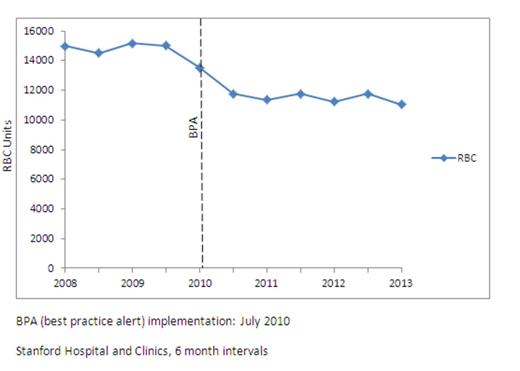
A clinical effectiveness team from key clinical services developed a consensus with a suggested transfusion threshold of hemoglobin (Hgb) 7 g/dl, or 8 g/dl for patients with acute coronary syndromes. Implemented in 7/2010, orders for RBC units triggered an interruptive BPA above a Hgb threshold of 7 g/dl for patients otherwise not excluded from the guidelines (according to their problem list: acute coronary syndrome, status post cardiothoracic procedure, hemorrhage, or hemodynamic instability). The BPA contained the consensus guidelines, link to relevant literature, and an “acknowledgement” reason if provider chose to continue transfusion. Trends in hospital-wide RBC utilization and clinical patient outcomes were analyzed for all in-patients discharged from January 2008 through December 2012.
The Figure shows impact on RBC utilization, before and after the BPA was implemented. RBC transfusions decreased substantially in the interval immediately after July 2010, and have continued to decrease thereafter. For 2012 compared to 2009, total RBC transfusions decreased by 24% (p < 0.05). This decrease in utilization has occurred despite concurrent increases in patient discharge volumes, case mix complexity, volumes of elective surgeries, and organ transplantation cases (Table). Additionally, patient clinical outcomes including mortality, length of stay, and 30 day readmission rates have declined or remained stable. For a subgroup of stable inpatients, the percentage of those receiving RBC transfusions when hemoglobin exceeded 8 g/dl, decreased from 57-66% preceding the CDS to 35% after (p=0.02); for the most recent interval, only 27% of RBC transfusions occurred outside guidelines. Comparing 2009 to 2012, total RBC transfusions decreased by 7,186 units, or 24%. Compared to purchase costs in 2009, for 2012 the estimated net savings (at $225/unit) in purchase costs was $1,616,850. Total net savings for 2010-2012 was $4,308,300.
We have substantially decreased RBC transfusions through real-time CDS, despite increasing volumes of health care delivery (patient discharges, elective surgeries, organ transplantation) and increasing complexity of case mix index. Moreover, hospital-wide patient quality indicators have been stable (mortality, 30 day readmission rates) or are improving (length of stay). CDS can be very effective for healthcare institutions to improve quality of care by simultaneously decreasing patient exposure to unnecessary RBC transfusion and by decreasing RBC supply costs along with the substantial transfusion-related costs.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.