Abstract
Data on pregnancy-associated acute myeloid leukemia (PA-AML) are scanty, coming from case reports and very small retrospective case series. The aim of the current study was to analyze reported maternal and fetal clinical characteristics and treatment decisions and provide a comprehensive basis for the development of guidelines for the management of women with PA-AML.
A systematic search of articles on PA-AML diagnosed during pregnancy or immediately after delivery, published between January 1967 and June 2013 in journals indexed in PubMed, was performed. Search terms of “acute leukemia”, “acute myeloid leukemia” and “acute promyelocytic leukemia” (APL) were crossed with terms “pregnancy”, “gestation” and “partum”. Additional potentially relevant reports referenced in reviewed articles were evaluated. Data on women's age, gestational stage, AML subtype, therapy, timing of its application, achieving complete remission (CR), survival status and fetal outcome (malformations, survival, birth weight) were recorded.
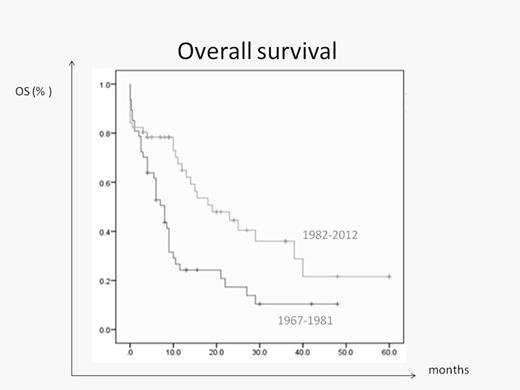
One hundred and seventy three PA-AML cases, reported in 88 papers, were analyzed. AML was reported in 120 cases (69%) and APL in 53 cases (31%). The French-American-British (FAB) AML categorization, available for 59 non-M3 AML cases, showed the distribution of AML subtypes similar to that reported in non-pregnant women (M1 - 3%, M2 - 12%, M4 - 30%, M5 - 27%, M6 - 5%, M7 - 1%). Median age at diagnosis was 28 years (range 15-45). Thirty seven women (22%) were diagnosed during 1st trimester, 85 (50%) in 2nd and 47 (28%) in 3rd trimester. The trimester was not reported in 4 cases. One hundred and twenty five women received chemotherapy during pregnancy: 18 in whom therapy was started in 1st trimester, 81- in 2nd and 26 - in 3rd trimester. In 46 patients, treatment was administered either after elective abortion (n = 26), or after delivery of a live baby (n =20). Data on therapy were unavailable in 2 cases. Delay in therapy beyond 1 week (range 2-20) from diagnosis (n = 21) did not affect the overall survival (OS) compared to that obtained in women treated promptly (median 11.5 vs 10.5 months, respectively; p=0.572). Among patients for whom remission data were available (n=151), 82 (73%) treated during pregnancy, and 27 (70%) treated after delivery, achieved CR. Within a median follow-up of 9 months (range 0-300), median OS for the entire cohort was 10.5 months (9 for AML vs 15.5 for APL; p=0.001). A multivariate analysis showed APL to be the only independent predictive factor for an improved OS (p=0.037), while maternal age and treatment delay had no statistically significant impact on OS (p= 0.83 and 0.889, respectively). Notably, the OS of women with PA-AML tended to improve over time (19 months for women treated over the last 30 years vs 8 months for those treated earlier; p = 0.09) (Figure 1); however, it is still less than the median OS of 3 years reported in age-matched non-pregnant women (http://seer.cancer.gov). One hundred and forty seven pregnancies were evaluable for the fetal outcome (excluding elective abortions); 117 (80%) pregnancies ended in delivery of a live baby. Six pregnancies where fetuses were exposed to chemotherapy during the 1st (n=1) or 2nd (n=5) trimester resulted in delivery of malformed newborns; 28 pregnancies ended in fetal death (5 stillbirths, 13 intrauterine fetal deaths, 4 post-delivery deaths, 5 unplanned abortions, 1 cause unavailable). Fetal outcome was unavailable for 2 babies. The median birth weight was 2.3 Kg for the 89 babies with reported weight (range 1.7-5 Kg). Among the 83 babies for whom data about birth weight and pregnancy week were available, 59% had a weight appropriate for the gestational age, 30% were small for gestational age and 11% were large for gestational age. In 89% of cases where information was available, the delivery was pre-term. No case of fetal leukemia was reported.
Based on our retrospective analysis, the outcome of women diagnosed with AML during pregnancy appears to be worse than that reported in age-matched non-pregnant women. The survival rate of the fetuses exposed to chemotherapy is encouraging. The incidence of malformations is low and the birth weight of most newborns is appropriate for the gestational age. Therapy delay could be considered in some of these patients, but large registry-based studies are warranted to establish treatment recommendations for the management of PA-AML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.