Abstract
Primary bone lymphoma (PBL) is a rare disease, representing approximately 7% of malignant bone tumors and 5% of extranodal lymphomas. There is inconsistent data in the literature regarding to definition, stage and prognostic factors. This study aims to describe our institutional experience in comparison with literature to identify any additional potential prognostic indicators.
Following the guidelines of Institutional Review Board, we retrospectively reviewed PBLs at Moffitt Cancer Center from 1998 to 2013 using data from medical record, Cancer Registry, and the Social Security Death Index. The pathological diagnosis was confirmed by experienced study pathologists using WHO classification. Clinical and radiological information was confirmed by study oncologists.
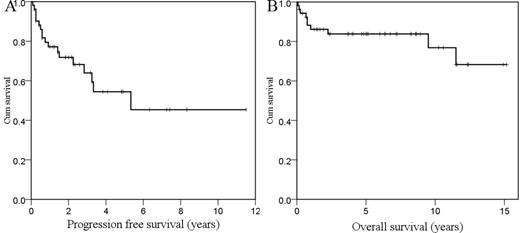
70 PBLs were included into our study, and most (n=53, 75.7%) were histologically classified as primary bone diffuse large-cell lymphoma (PB-DLBCL) (Table 1. There was a slight male predominance (1.3:1) with a median age of 56.5 years (15-89). Femur, spine and pelvis were most commonly involved. Most patients present with local bone pain (88.5%). Soft tissue extension is common (55.8%). Multifocal bone lesions and Ann Arbor Stage IV disease were observed in 27 patients (38.6%) and 41 patients (44.3%), respectively. Of 70 PBLs, 38.6% were treated with combined modality therapy, 8.6% were treated with radiation therapy alone, and 48.6% were treated with chemotherapy alone. The data of PB-DLBCL subgroup were further analyzed for survival. The patients with PB-DLBCL had 3- and 5-year progression free survival (PFS) of 61.2% and 46.9% respectively, while 5- and 10-year overall survival (OS) were 81.1% and 74.7% (Figure 1 ). In univariate analysis, soft tissue extension (p=0.009), multifocal lesions (p=0.002), stage IV (p=0.001), elevated LDH (p=0.027), high International Prognostic Index (IPI) score (p<0.001), and single-modality therapy (p=0.004) were significant poor prognostic factors for PFS. Age ≥60 years (p= 0.012), soft tissue extension (p=0.015), multifocal lesions (p<0.001), stage IV (p=0.001), elevated LDH (p= 0.034), high Performance Score (p=0.036), high IPI score (p<0.001), and single-modality therapy (p=0.021) were significant poor prognostic factors for OS. Multivariate analysis revealed that soft tissue extension and IPI score were two independent prognostic factors for both PFS and OS in patients with PB-DLBCL (Table 2 ).
Histopathological subtypes of 70 patients with PBL
| Classification . | Number . | % . |
|---|---|---|
| DLBCL | 53 | 75.7 |
| FL | 7 | 10.0 |
| SLL | 2 | 2.9 |
| MZL | 1 | 1.4 |
| Unclassifiablea | 1 | 1.4 |
| Unclassifiableb | 2 | 2.9 |
| HL | 1 | 1.4 |
| T cellc | 3 | 4.3 |
| Total | 70 | 100.0 |
| Classification . | Number . | % . |
|---|---|---|
| DLBCL | 53 | 75.7 |
| FL | 7 | 10.0 |
| SLL | 2 | 2.9 |
| MZL | 1 | 1.4 |
| Unclassifiablea | 1 | 1.4 |
| Unclassifiableb | 2 | 2.9 |
| HL | 1 | 1.4 |
| T cellc | 3 | 4.3 |
| Total | 70 | 100.0 |
a Unclassifiable B-cell lymphoma with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma
b Unclassifiable low grade B-cell lymphoma
c T-lymphoblastic lymphoma (n=1), anaplastic large cell lymphoma (n=2). Abbreviations: DLBCL, diffuse large B-cell lymphoma; FL, follicular lymphoma; SLL, small lymphocytic lymphoma; MZL, marginal zone lymphoma; HL, Hodgkin's lymphoma.
Progression free survival (A) and overall survival (B) of 53 patients with PB-DLBCL
Progression free survival (A) and overall survival (B) of 53 patients with PB-DLBCL
Multivariate analysis of prognostic factors for patients with PB-DLBCL
| Parameter . | PFS . | OS . | ||||
|---|---|---|---|---|---|---|
| RR . | 95%CI . | p . | RR . | 95%CI . | p . | |
| Soft tissue extension | ||||||
| No | 0.274 | 0.089-0.848 | 0.025 | 0.072 | 0.007-0.752 | 0.028 |
| Yes | Reference group | Reference group | ||||
| IPI group | 0.003 | 0.001 | ||||
| Low (0-1) | 0.057 | 0.011-0.305 | 0.001 | 0.008 | 0.000-0.150 | 0.001 |
| Intermediate(2-3) | 0.465 | 0.155-1.400 | 0.173 | 0.117 | 0.027-0.530 | 0.004 |
| High(4-5) | Reference group | Reference group | ||||
| Parameter . | PFS . | OS . | ||||
|---|---|---|---|---|---|---|
| RR . | 95%CI . | p . | RR . | 95%CI . | p . | |
| Soft tissue extension | ||||||
| No | 0.274 | 0.089-0.848 | 0.025 | 0.072 | 0.007-0.752 | 0.028 |
| Yes | Reference group | Reference group | ||||
| IPI group | 0.003 | 0.001 | ||||
| Low (0-1) | 0.057 | 0.011-0.305 | 0.001 | 0.008 | 0.000-0.150 | 0.001 |
| Intermediate(2-3) | 0.465 | 0.155-1.400 | 0.173 | 0.117 | 0.027-0.530 | 0.004 |
| High(4-5) | Reference group | Reference group | ||||
Our institutional experience confirms, although PB-DLBCL comprises the majority of PBL, the overall prognosis of PBL is good. In PB-DLBCL, soft tissue extension and higher IPI score are associated with an inferior OS and PFS. The authors emphasized that prognostic significance of soft tissue extension and IPI in PBL are not well discussed in the literature, which warrants further investigation in larger well-characterized clinical cohorts.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.