Abstract
Bronchiolitis Obliterans Syndrome (BOS) is a late-onset non-infectious pulmonary complication of HSCT, resulting in obstructive lung disease. BOS is thought to be a manifestation of chronic graft versus host disease (cGVHD). BOS can also occur after lung transplantation, where it is believed to represent chronic rejection of the lung allograft. In both conditions, the mainstay of therapy includes augmentation of systemic immunosuppression. However, this approach has limited efficacy and is associated with deleterious consequences including an increased risk of infection and decreased graft versus tumor/leukemia effects. We investigated whether targeted, local delivery of inhaled cyclosporine could improve or stabilize lung function in BOS patients.
HSCT recipients with BOS, ages 10-80, were eligible if they met the following inclusion criteria: FEV1<75% predicted, FEV1 decline >10% compared to pre-transplant FEV1, no evidence of pulmonary infection as a causative etiology, and one of the following: FEV1/FVC ratio <70%, air-trapping seen on CT scan or RV ≥120%, or evidence of cGVHD affecting at least one other organ system. Lung transplant recipients with BOS were also eligible. Subjects were characterized as having progressive or stable disease at study entry based on their FEV1 values in the preceding 3-18 weeks. Progressive disease was defined as a ≥10% decline in FEV1, and stable disease as an increase in FEV <5% or a decrease <10%. Subjects received cyclosporine inhalation solution (CIS) 150 mg via nebulizer 3 times weekly for 6 weeks before dose escalation to 300mg three times weekly. The primary endpoint was change in FEV1 at study completion (average of week 18 and 19 values) compared to study baseline. Pharmacokinetic sampling and lung deposition studies were performed on all subjects. Lung deposition studies were performed using SPECT/CT imaging after inhalation of CIS mixed with technetium- 99m sulfur colloid. Bronchoalveolar lavage fluid and peripheral blood samples were collected at study baseline, week 9 and week 18, and were analyzed for cytokine markers and lymphocyte phenotype. Six minute walk tests (6MWT) and quality of life testing was also performed.
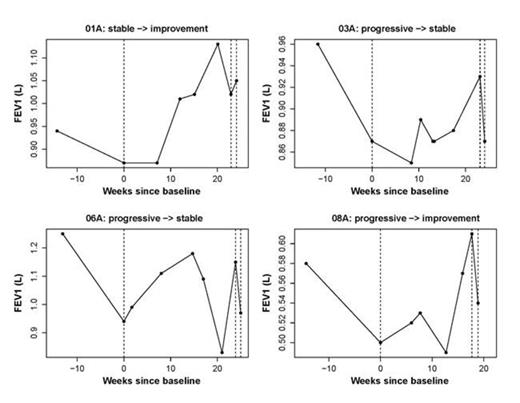
Eleven subjects (nine evaluable) have been enrolled (median age: 45 years; range: 14-73). Nine subjects had HSCT-associated BOS, and 2 had lung-transplant-associated BOS. Patients were transplanted for various underlying conditions (MDS, aplastic anemia, DLBCL, MM, ALL, Gata-2 deficiency, alpha-1 anti-trypsin deficiency, and idiopathic pulmonary fibrosis). HSCT recipients received both reduced intensity (n=4) and myeloablative (n=5) conditioning, with allografts from HLA matched relatives (n=5) or unrelated donors (n=4). The median time from BOS diagnosis to study enrollment was 9 months (range: 2-37 mos). The median FEV1 at study entry was 1.11 liters (range: 0.5-2.11), with 4 subjects having progressive disease and 7 stable disease. Adverse events associated with CIS occurred in 9/10 patients and included cough, bronchospasm, and dyspnea. Most adverse events were grade 2 (range:1-3) and occurred only during the inhalation.
Three subjects went off-study (patient choice) prior to completion of the 18 weeks due to adverse events and were considered non-responders. Four of the 8 (50%) HSCT- associated BOS subjects had a response, including 3 patients with progressive disease and 1 with stable disease at study entry. Among these responders, the improvements in absolute FEV1 from baseline were 19.5%, 15%, 12.7%, and 3.4% respectively (figure). Among the responding patients, 2 were also able to decrease their systemic steroid administration by 50% and 43%. An improvement in 6MWT was noted in 1/4 responders. Four responders have enrolled onto an extension protocol.
The median peak systemic absorption of cyclosporine was 99 mcg/L (Range: 32-263) 20 minutes post-CIS inhalation. Lung deposition studies showed the total deposited dose averaged 12% (range: 4-20 %) of the inhaled dose.
Inhaled cyclosporine can be delivered safely and can stabilize or improve lung function in HSCT recipients with severe BOS, allowing systemic immunosuppression to be reduced. Use of local, targeted therapy with CIS resulted in minimal systemic absorption compared to typical oral administration, and achieved high drug levels in the lung tissue as demonstrated by the lung deposition results.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.