Abstract

Children with sickle cell anemia (SCA) have a high risk of stroke that can be estimated by transcranial Doppler ultrasonography (TCD). The gold standard TCD measurement to determine the risk of primary stroke is the time-averaged mean of the maximum velocity (TAMMV) in specific intracranial arteries. Peak systolic velocity (PSV), a different TCD measurement, has been proposed as an alternative method for risk stratification, especially for imaging TCD (TCDi) techniques (Jones et al. 2005). Although PSV has been little studied for this purpose, some centers use PSV in addition to TAMMV for the classification of risk of stroke by TCD for clinical care. A systematic bias in the classification of risk of stroke by PSV (higher or lower compared to TAMMV) would substantially affect medical resources and patient outcomes.
Describe the test performance characteristics of PSV compared to TAMMV for the classification of risk of stroke in children with SCA and determine the suitability of PSV for classification of TCDs in clinical practice.
We studied all patients in our center with homozygous HbSS, sickle-β0-thalassemia, or sickle-Hb D disease (all genotypes referred to here as SCA) who were ≥2 years of age and had a clinical TCD (all by TCDi technique) between 1998-2013. For each patient, the single most recent TCD performed >30 days from a transfusion was used, except for patients receiving chronic transfusions for whom the TCD before the initiation of chronic transfusions was used. Patients were included only once in this analysis. The highest TAMMV and PSV were recorded for the distal internal carotid artery (DICA), bifurcation and middle cerebral artery on the right and left sides of the brain. The TAMMV in each vessel was classified using modified STOP velocity criteria for TCDi: <155, normal; 155-184, conditional; ≥185 abnormal. The PSV in each vessel was classified using criteria proposed by Jones et al.: <200, normal; 200-249, conditional; ≥250 abnormal. Two overall TCD classifications, using either TAMMV or PSV, were made according to standard STOP methods by considering the worst (most abnormal) classification of any vessel as the overall classification. The primary outcome was the multi-level agreement between overall TCD classification based on TAMMV and PSV as measured by the kappa statistic. Kappa was also calculated for individual vessels to determine if agreement differed by anatomic site. Coefficients of determination (r2) were calculated using Pearson correlation.
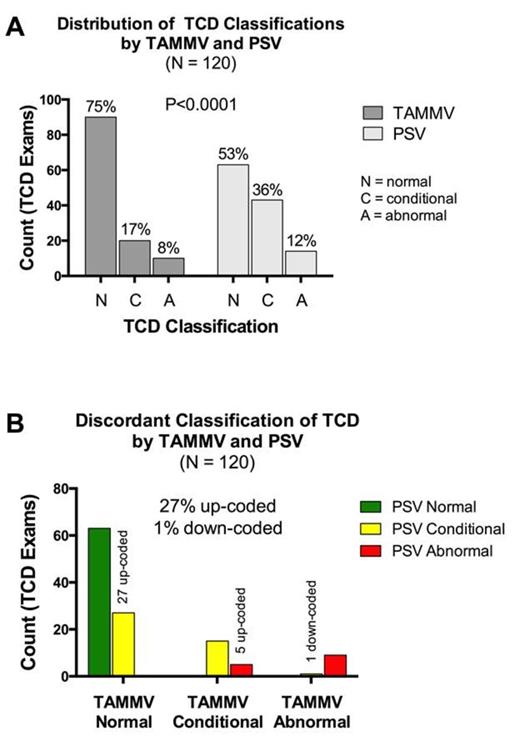
We studied 120 patients with SCA [mean age 12.0 years ± 6.0 (S.D.); 51.1% male]. Fifty-nine (49%) had at least one prior transfusion that was given a mean of 588 (median 387) days before the TCD (none ≤40 days). The distribution of overall TCD classification by simultaneous TAMMV and PSV is shown in the Figure (Panel A). The distribution of classifications by TAMMV, compared to PSV, better approximates the expected distribution in a screening population. Classifications by PSV were skewed higher, giving more conditional and abnormal results, when compared to classification by TAMMV (P<0.0001). Kappa was 0.488 (P<0.001) for overall TCD classification, indicating only moderate agreement between the TAMMV and PSV methods. Agreement between TAMMV and PSV classification was highest (“substantial”) in the right and left DICA (k: 0.657–0.717, P<0.001). Agreement was only moderate in all other vessels (k: 0.428–0.539, P<0.001). Compared to TAMMV, use of PSV resulted in misclassification of 28% of overall TCD interpretations (Figure, Panel B); 32 studies (27%) were up-coded (27 normal to conditional; 5 conditional to abnormal). Only 1 study was down-coded (abnormal to conditional). Considering TAMMV and PSV as continuous variables, TAMMV accounted for 84.2-90.2% (r2) of the variation in PSV across different vessels; so, approximately 10-15% of the variability in PSV is not explained by TAMMV.
The use of PSV (rather than TAMMV) to classify TCDs overestimates the risk of stroke for almost one-third of children with SCA. This systematic bias will unnecessarily increase anxiety, the frequency of follow-up testing, and use of chronic transfusions for primary stroke prophylaxis. PSV should not be used for primary classification of TCDs in clinical practice.
Jones A et al. Can peak systolic velocities be used for prediction of stroke in sickle cell anemia? Pediatr Radiol. 2005;35:66-72.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract