Abstract
Human mesenchymal stem cells (MSCs) can be isolated from several tissues, including bone marrow, umbilical cord, placenta, and adipose tissue. In recent reports, MSCs have the ability to migrate to inflammatory tissues and suppress adverse immune reactions. In fact, BM-derived MSCs are already applied for the patients with acute graft versus host disease (aGVHD) with promising efficacy. To avoid the potential risk of BM harvest, we intended to use umbilical cord Wharton's jelly (WJ) as an alternative source for MSCs. However, the mechanism by which WJ-MSCs exert their immunosuppressive effects is not completely understood.
Umbilical cord was collected after informed consent from the mother. WJ-MSCs were isolated by explants method and in part, continued to culture for further expansion by passage 3 (P3). Otherwise, the remaining WJ-MSCs were cryopreserved in P1. Mixed lymphocyte reaction (MLR) was performed on WJ-MSCs or control. CFSE-labeled human peripheral blood (PB) or cord blood(CB) derived mononuclear cells (MNCs) as the responder cells were mixed with irradiated (50Gy) human CB-derived dendrite cells as stimulator cells at a 10:1 ratio, in the presence of low-dose anti-CD3 antibody. CFSE-labeled responder cells were analyzed by FACS.
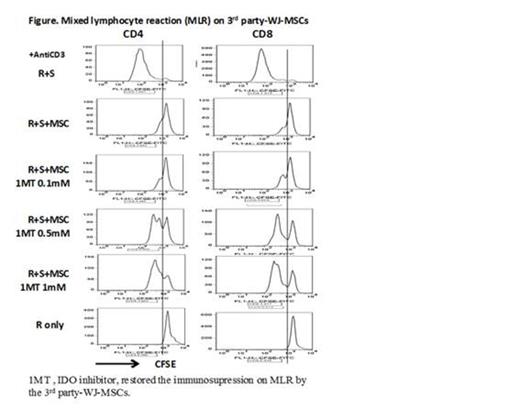
WJ-MSCs corresponded to the minimal criteria of MSCs defined by the International Society for Cell Therapy. Thus WJ-MSCs showed spindle-shaped plastic adherent with positive CD105, CD73, CD90, and negative for CD45, CD34, CD14, CD19, and HLA -DR. They also have the ability of differentiation into osteoblasts, adipocytes, chondroblasts in vitro. In MLR, WJ-MSCs efficiently inhibited the responder T cells derived from the same donor of WJ-MSCs, triggered by autologous or allogeneic dendritic cells (DC)(Autologous and allogeneic MLR). Moreover, 3rd party-derived WJ-MSCs also strongly suppressed allogeneic responder T cells proliferation triggered by allogeneic DC(3rd party MLR) (n=3). And WJ-MSCs could inhibit the proliferation of T cells upon PHA-L stimulation. In order to study whether the inhibitory effects of WJ-MSCs on MLR requires the cell to cell contact or not, we next performed MLR on separated WJ-MSCs using by transwell. We observed the inhibitory effect of WJ-MSCs on MLR, although the immunosuppressive effect of the separated WJ-MSCs was much less than that of cell to cell contact. The supernatants of WJ-MSCs, which were derived from 80% confluent WJ-MSCs indicated the mild inhibitory effects on MLR. These inhibitory effects of the WJ-MSCs on MLR were reversed by the addition of indoleamine 2,3-dioxygenase (IDO) inhibitor, 1-methyltryptophan (1-MT) , in a dose dependent manner as shown in Figure 1 (n=3). We also studied the influence of the passage of WJ-MSCs on MLR. The inhibitory effect was comparable among the early passage (∼P3) and long-term passage (P10), although the long-term passage did not show the osteogenic differentiation.
We demonstrated WJ-MSCs have the immunosuppressive effect on the stimulated T cells in autologous, allogeneic and 3rd party MLR setting, indicating that immunosuppressive effect of WJ-MSCs is not restricted by MHC. Soluble IDO may play an important role in immunosuppressive effect of MLR, although we need to detect the additional factors especially in cell to cell contact between WJ-MSCs and the responder T cells. Conclusively, WJ-MSCs may be a feasible alternative non-invasive source of BM-MSCs for GVHD treatment and WJ-MSCs banking can be considered for the prompt clinical applications.
No relevant conflicts of interest to declare
Author notes
Asterisk with author names denotes non-ASH members.

