Abstract
Possibilities to monitor the intensity of dabigatran etexilate (DE) treatment may be valuable before urgent intervention. The Working Group on Perioperative Haemostasis proposed that the drug plasma concentration ([]) should be less or equal to 30ng/mL. However, plasma levels where it is safe to carry out an invasive procedure or surgery have not been confirmed prospectively. In addition, no biological test has been correlated with bleeding risk. Literature showed heterogeneous data regarding the arrest of DE depending on the renal function and the haemorrhagic risk. In addition, physicians request guidance for patients excluded from the clinical trials. Consequently, there is still a need for a rapid and widely available biological test.
Some authors make proposals based on activated Partial Thromboplastin Time (aPTT), Hemoclot Thrombin Inhibitor® (HTI) or Thrombin Time (TT). TT displayed several advantages over aPTT. However, TT is affected by numerous analytic variables.
Therefore, the objectives of the present study were:
1. To determine the optimal [thrombin] with a variety of instruments and reagents
2. To assess the repeatability of TT at optimized conditions
3. To compare the sensitivity and linearity of TT at residual [dabigatran] (DA) with those of aPTT and HTI
4. To validate the fibrinogen reagent (with heparin inhibitor) for TT experiments
DA was spiked at increasing [] in pooled citrated normal human platelet-poor plasma (NPP). The following [DA] were prepared: 0, 5, 10, 20, 30, 40 and 50ng/ml.
1. Optimal [thrombin] determination.
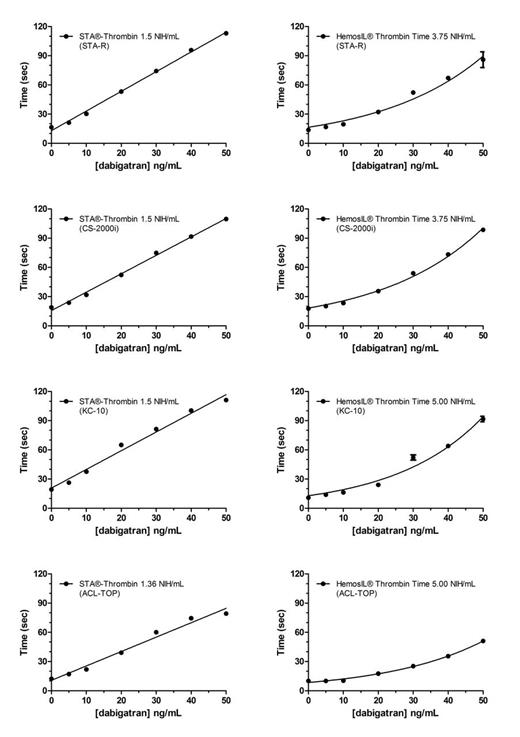
The optimal [thrombin] was defined with 2 reagents: bovine thrombin (HemosIL® TT) and human thrombin (STA®-Thrombin) on 4 instruments: STA-R Evolution®, ACLTOP® , CS2000i® and KC10®.
TT higher than Tmax is not informative for the physician. Thus the optimized [thrombin] was defined as the maximum [] giving, in a reproducible way, a TT at 50ng/ml lower than Tmax and a TT at 0ng/ml higher than the minimum TT. The Tmax was set arbitrarily at 120 sec.
2. Repeatability
The repeatability of optimized TT was assessed by running aliquots of NPP spiked with all [DA] on 10 consecutive days
3. TT (1.5 NIH/ml, STA®-Thrombin), aPTT with SynthasIL® and STA®-C.K.Prest, and HTI were also determined within 1 hour on STA-R® on replicates of all NPP solutions.
4. STA®- Fibrinogen-5 was diluted to the optimized [thrombin] (1.5 NIH/ml) on STA-R® and used as a thrombin reagent.
1. The thrombin origin is a more important variable in comparison to the type of coagulometer. At [DA] of 30ng/ml and [thrombin] of 1.5 NIH/ml, the STA®-TT ranges from 56 sec to 74 sec according to the instrument, whereas on a same instrument, the TT varied of minimum 43 sec, depending on the thrombin origin.
The optimized [thrombin] are the following : a) STA-R®, STA®-Thrombin : 1.5 NIH/ml, b) STA-R®, HemosIL® TT : 3.8 NIH/ml, c) ACLTOP®, STA®-Thrombin 3.8 NIH/ml, d) ACLTOP®, HemosIL® TT 5.0 NIH/ml, e) KC10®, STA®-Thrombin 1.5 NIH/ml, f) KC10®, HemosIL® TT 5.0 NIH/ml, g) CS2000i®, STA®-Thrombin 1.4 NIH/ml, h) CS2000i®, HemosIL® TT 3.8 NIH/ml.
Except for STA®-Thrombin on STA-R®, the [optimized] is not the one recommended by the manufacturer. Figure 1 shows the results of optimized TT according to thrombin origin and coagulometer.
2. Repeatability experiments showed that variability increased with the [DA] (i.e. STA®-Thrombin (STA-R®): coefficient of variation: 8.0% and 28.9% for 0ng/ml and 50ng/ml, respectively) and that the variability depends on the coagulometer and the reagent.
3. Comparison of sensitivity and linearity of TT, aPTT and HTI are presented in Table 1. APTT is not sensitive enough in low [DA], whatever the reagent, whereas HTI is not suitable in [DA] lower than 50ng/ml.
3. TT performed with fibrinogen reagent shows longer times in comparison to thrombin reagent (>120 sec vs 109 sec at 30ng/ml DA).
| [Dabigatran] (ng/ml) . | TT (sec) . | aPTT (sec, SynthasIL®) . | aPTT (sec, STA®-C.K.Prest) . | HTI (ng/ml) . |
|---|---|---|---|---|
| 0 | 17.9 | 30.3 | 31.2 | 0.0 |
| 5 | 22.0 | 31.2 | 33.1 | 0.0 |
| 10 | 31.5 | 32.4 | 34.5 | 0.0 |
| 20 | 59.3 | 34.9 | 38.6 | 7.2 |
| 30 | 82.9 | 36.0 | 39.6 | 10.3 |
| 40 | 100.9 | 38.0 | 42.8 | 21.3 |
| 50 | 120.0 | 39.3 | 44.2 | 27.4 |
| [Dabigatran] (ng/ml) . | TT (sec) . | aPTT (sec, SynthasIL®) . | aPTT (sec, STA®-C.K.Prest) . | HTI (ng/ml) . |
|---|---|---|---|---|
| 0 | 17.9 | 30.3 | 31.2 | 0.0 |
| 5 | 22.0 | 31.2 | 33.1 | 0.0 |
| 10 | 31.5 | 32.4 | 34.5 | 0.0 |
| 20 | 59.3 | 34.9 | 38.6 | 7.2 |
| 30 | 82.9 | 36.0 | 39.6 | 10.3 |
| 40 | 100.9 | 38.0 | 42.8 | 21.3 |
| 50 | 120.0 | 39.3 | 44.2 | 27.4 |
TT may be more informative than aPTT and HTI to provide with guidance to carry out an urgent procedure or surgery for patients receiving DE. However, TT is affected by a lot of analytic variables that should be understood by laboratories. Each laboratory should optimize its TT procedure according to its combination coagulometer-reagent.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.