Abstract
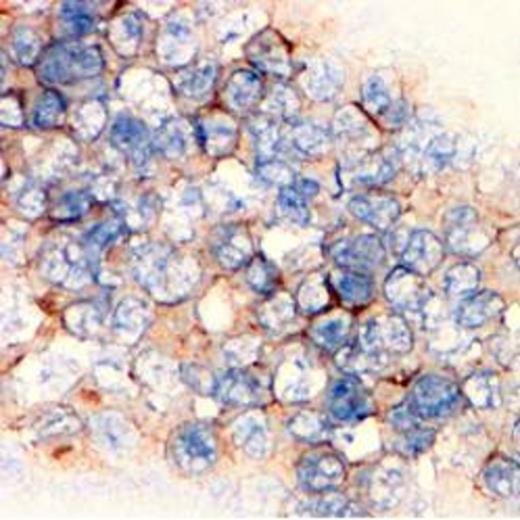
The pathogenesis of MDS is multifactorial including both cell intrinsic alterations, such as mutations, and cell extrinsic stimuli such as immune deregulation. The prognosis of patients that lose response to hypomethylating agents (HMAs) is very poor and the mechanisms are not understood. Leukemia cells develop multiple resistance mechanisms to escape host immune response. Programmed death-1 (PD-1) is a negative costimulatory receptor on activated T lymphocytes. Expression of PD-1 ligands on tumor cells can induce immunosuppressive T-cells. Recent studies have indicated that demethylation of PD-1 leads to exhausted CD8+ T cells after chronic virus infection. We hypothesized that dysregulated PD-1 immune checkpoint signaling may be involved in pathogenesis of MDS and resistance to HMAs. We first evaluated the mRNA expression levels of PD-L1, PD-L2, PD-1 and CTLA4 by Q-PCR in bone marrow CD34+ cells from 124 patients which include 69 with MDS, 46 with CMML and 9 with AML. Seventy two (58%) patients were previously untreated. We observed aberrant up-regulated mRNA expression of PD-L1 in 39 patients (34% with fold 0-843.3), PD-L2 in 17 patients (14% with fold 0-22.5), PD-1 in 18 patients (15% with fold 0-76.7) and CTLA4 in 10 patients (8% with fold 0-25.1). No significant differences in gene expression were observed when comparing patients that had and had not received prior therapy. Statistically significant relationships were identified between elevated PD-1 expression and increased age (p=0.008), while elevated PD-L2 expression correlated significantly with female gender (p=0.005). Both elevated PD-L1 and CTLA4 expression correlated with MDS subtype, (p=0.034) and (p=0.012), respectively. Additionally, elevated CTLA4 expression correlated with higher white blood cell count (p=0.021), lack of prior therapy (p=0.02) and lower MDS IPSS score (p=0.027). We then performed an analysis of the impact on survival of the 4 gene expression in patients that had not received prior therapy. Patients with lower expression of PD-L1 had a non-significant trend towards better survival (31.5 months versus 16.2, p=0.24). Forty six of 124 patients analyzed received HMAs, and within these 46 patients lower PD-L1 expression correlated with a significantly improved overall response rate (67% vs 25%, p=0.038). Aberrant up-regulation of these 4 genes was also observed in peripheral blood mononuclear cell (PBMNC) from 61 MDS, CMML and AML patients. The relative expression of PD-L1 was significantly higher in MDS (p=0.018) and CMML (p=0.0128) compared to AML. Of interest, mRNA expression of these 4 genes was significantly higher in PBMNC than in CD34+ cells except PD-L1. By immunohistochemical (IHC) analysis, a strong correlation was observed between protein and mRNA expression. By IHC, we observed that leukemia blasts were positive for PD-L1 whereas stroma/non-blast cellular compartment was positive for PD-1 in bone marrow biopsies from MDS, CMML and AML patients. We then analyzed effect of HMAs on these four gene expression in cohort of 61 patients treated with different trials of epigenetic therapy. Treatment resulted in up regulated expression of PD-L1 in 57% of the patients (with maximum induction fold of 4.8), PD-L2 in 57% (maximum fold of 15.77), PD-1 in 58% (maximum fold of 50.26) and CTLA4 in 66% (maximum fold of 29.9). Of importance, patients resistant to therapy had increased gene expression compared to patients that achieved response (fold 5.3 vs 0.4 for PD-L1, 6.2 vs 0.4 for PD-L2, 3.0 vs 0.4 for PD-1 and 5.4 vs 0.7 for CTLA4). Comparing patients without and with expression induction, the median survival was 11.7 and 6.6 months (p=0.122) for PD-L1, 12.5 and 4.7 months (p=0.029) for PD-L2, indicating a better prognosis in patients without PD-L1 and PD-L2 induction treated with HMAs. To model this observation, we treated KG-1 and THP1 cells with different concentrations of decitabine (0 to 10 uM) and observed a dose dependent up-regulation of PD-L1 and PD-L2 in THP1 cells, and CTLA4, PD-1, PD-L1 in KG1 cells. Exposure to decitabine resulted in demethylation of PD-1 in these cell lines, and the demethylation effect was also observed in HMAs treated MDS and AML patients. This study suggests immune checkpoint PD-1/PD-1 ligands signaling may be involved in MDS pathogenesis and resistance mechanisms to HMAs. Blockade of this pathway can be a potential therapy in MDS and AML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.