Abstract
The association between malignancy and venous thromboembolism (VTE) is well established. Less is known about the independent impact of VTE, both symptomatic and incidental, on survival in patients with prostate cancer.
We conducted a retrospective cohort study of 457 consecutive patients with prostate cancer who received outpatient clinical care at the Cleveland Clinic from January 2006 to June 2006. Data were collected regarding clinical characteristics, treatment and outcomes. Fisher exact (for categorical variables) and t-test (continuous variables) were utilized to test associations with VTE and mortality. Survival functions were estimated using the Kaplan Meier method and a Cox regression model was used to model the mortality hazard ratio (HR) with date of diagnosis as time origin.
The mean age of our cohort of patients was 65.86 ± 8.64 years. Three hundred and fifty eight (78.3%) had clinically localized disease, 76 (16.7%) had locally advanced disease and 41 (8.9%) had metastatic cancer at diagnosis. One hundred twenty four (27.1%) men underwent surgery, 315 (68.9%) received radiotherapy, 201 (44%) received hormonal therapy and 71 (15.5%) received chemotherapy. Complete follow up was available on 403 patients of which 109 (27%) died during the period of follow up. VTE occurred in 42 (9.2%) patients (33 deep vein thrombosis, 5 pulmonary embolism, and 4 patients with both DVT and PE), of which 27 (64.3%) were symptomatic and 15 (35.7%) were incidentally diagnosed. Twenty-three were outpatients and 17 were hospitalized when VTE was diagnosed. Metastatic disease (p<0.0021), and chemotherapy (p=0.002) were associated with VTE. There was no association of VTE with more traditional risk factors such as obesity, renal disease, rheumatologic disease, hip fracture, COPD, and smoking.
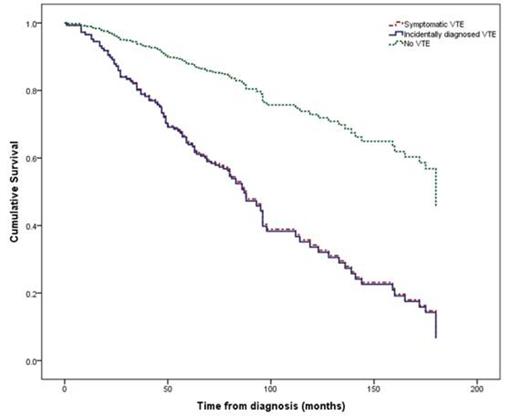
Metastatic disease (p=0.002), ECOG score of 3 or 4 (p<0.001), and VTE (p<0.001) were predictors of mortality. Adjustment for stage of disease was included in the multivariate analysis. Mean survival of patients with and without VTE was 91.8±11.3 months and 144.8±3.6 months respectively (p<0.01). Five-year survival rates were also significantly lower for patients with VTE compared to those without (45.2% vs. 87.8%, p<0.001). Patients with both symptomatic and incidental VTE had significantly poorer survival than those without however there was no significant difference in survival between patients with symptomatic or incidental VTE (70.78±44.82 years versus 77.87±63.07, p=0.674).
VTE, both symptomatic and incidental, is a predictor of poor survival in patients with prostate cancer, especially those with advanced disease. This finding has implications for the clinical care of patients with prostate cancer. Further studies are needed to evaluate the benefit of prophylactic and therapeutic anticoagulation in this population.
Characteristics of patients with prostate cancer who developed venous thromboembolic disease (VTE)
| Patients who developed VTE . | N = 42/403 (9.2%) . |
|---|---|
| Age | |
| Stage Limited stage Locally advanced disease Metastatic disease | 4 10 28 |
| ECOG performance status 0 1 2 3 4 | 4 (9.5) 12 (28.6) 6 (14.3) 11 (26.2) 4 (9.5) |
| Type of presentation DVT PE Both DVT and PE | 33 (78.6) 5 (11.9) 4 (9.5) |
| Location of DVT Upper extremity (Jugular, subclavian, axillary) Ilio-femoral Popliteal Inferior vena cava Bilateral upper extremity Bilateral lower extremity | 2 19 12 4 1 6 |
| Symptomatic VTE Incidentally diagnosed VTE | 27 (64.3) 15 (35.7) |
| Clinical setting Inpatient Outpatient | 17 (40.5) 25 (59.5) |
| Central line associated DVT | 1 (2.4) |
| Patients who developed VTE . | N = 42/403 (9.2%) . |
|---|---|
| Age | |
| Stage Limited stage Locally advanced disease Metastatic disease | 4 10 28 |
| ECOG performance status 0 1 2 3 4 | 4 (9.5) 12 (28.6) 6 (14.3) 11 (26.2) 4 (9.5) |
| Type of presentation DVT PE Both DVT and PE | 33 (78.6) 5 (11.9) 4 (9.5) |
| Location of DVT Upper extremity (Jugular, subclavian, axillary) Ilio-femoral Popliteal Inferior vena cava Bilateral upper extremity Bilateral lower extremity | 2 19 12 4 1 6 |
| Symptomatic VTE Incidentally diagnosed VTE | 27 (64.3) 15 (35.7) |
| Clinical setting Inpatient Outpatient | 17 (40.5) 25 (59.5) |
| Central line associated DVT | 1 (2.4) |
Survival curves depicting survival (in months) for patients without venous thromboembolic disease (VTE), symptomatic VTE and incidental VTE. Patients with VTE, both incidental and symptomatic, had significantly worse survival than those without (p<0.001). There was no significant difference in survival between patients with symptomatic and incidental VTE (p=0.674).
Survival curves depicting survival (in months) for patients without venous thromboembolic disease (VTE), symptomatic VTE and incidental VTE. Patients with VTE, both incidental and symptomatic, had significantly worse survival than those without (p<0.001). There was no significant difference in survival between patients with symptomatic and incidental VTE (p=0.674).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.