Abstract
Pathological lymphangiogenesis, consisting in the formation of new lymphatic vessels, is important for the development of tumors, including DLBCL. The VEGF-C/VEGF-D/VEGFR-3 axis is currently considered the main route of transmission for extracellular prolymphoangiogenic signals. The aim of our study was to assess the plasma levels of VEGF-C, VEGF-D and VEGFR-3 in DLBCL patients upon diagnosis, and the evolution of the above cytokines during the R-CHOP therapy in relationship to its outcome, as well as to evaluate the predictive value of cytokines as to the achievement of complete remission (CR), and their prognostic value regarding the overall survival (OS).
55 previously untreated DLBCL patients (38 M and 17 F), aged 23 - 88 yrs (average: 65.4 ±14.7), followed in the Holycross Cancer Center, Kielce, Poland, and 30 healthy control individuals (9 M and 21 F), aged 39 - 88 yrs (average: 61.1±11.9), were enrolled into the study.
The patients received 6-8 courses of the standard 21-R-CHOP regimen. 24 out of 55 (43,6%) patients, achieved CR, the remaining ones did not (NCR).
The cytokine concentrations in plasma of peripheral blood were established with the ELISA assay before treatment, after the 3rd or 4rd cycle and after the end of the treatment.
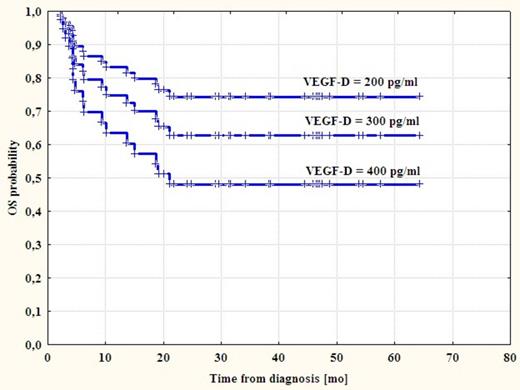
The results were processed statistically with the Mann-Whitney and the Wilcoxon paired sample tests, the Spearman rank correlation coefficient and the chi2 test. The “p” value of below 0.05 was assumed as statistically significant. In order to evaluate the influence of the cytokines concentration on the OS of patients using the Kaplan-Meier method, survival curves were designed and compared with the use of the log-rank test.
There was no significant relationship between gender and cytokines concentration in both patients and control group. VEGFR-3 plasma concentration was higher at diagnosis in the whole population of patients (75.8 ± 42.1 ng/ml), and in the CR and NCR groups assessed separately, compared to healthy subjects (45.7±16.7 ng/ml) (p=0.007; p=0.001; p=0.012; respectively for the whole population, CR and NCR group). VEGFR-3 in the whole population was significantly lower after the 3rd or 4rd cycle of R-CHOP than before treatment (65.0+31.0 ng/ml and 75.8±42.1 ng/ml respectively, p=0.03).
There were no significant differences in the VEGF-C and VEGF-D concentrations between whole population of untreated patients and control group. VEGF-C was lower after the end of treatment in comparison to the values after the 3rd or 4rd cycle in the whole population (2777.5 ± 1615.0 pg/ml and 2917.4 ± 1615.0 pg/ml, p=0.04) and in CR group (3100.9 ± 1549.7 pg/ml and 3379.4 ± 2535.4 pg/ml, p=0.03). VEGF-D in CR group before treatment was significantly lower than in healthy individuals (243.3 ± 117.7 pg/ml and 372.9 ± 178.6 pg/ml respectively, p=0.01). We found no other significant variations in concentrations of the cytokines studied during the course of treatment.
We observed a correlation between both VEGFR-3 and VEGF-D concentrations and the b2-microglobulin level (R=0.37, p=0.01 and R=0.35; p=0.02; respectively), significantly higher sVEGFR-3 and VEGF-C values for patients with IPI 3-5 than IPI 0-2 (p=0.048 and p=0.02; respectively), a positive correlation between VEGF-D concentration and LDH activity (R=0.35, p=0.01) as well as a negative correlation between VEGF-D and albumin concentration (R=-0.44, p=0.001).
The OS time was 3-54 months. The OS probability curves established according to Kaplan-Meier method did not significantly differ between patients with any evaluated cytokine concentration above and below the median value. However, Cox regression model showed negative prognostic impact of high VEGF-D concentration on OS (HR = 1.005, 95% CI 1.001-1.009, p=0.008)(Fig).
We failed to demonstrate a coherent pattern of the evolution of plasma concentrations of the cytokines involved in the lymphangiogenesis during the treatment of DLBCL. However, our results suggest that a release of some of them into the bloodstream may be tumor-dependent and related to its burden. Additionally, the negative impact of plasmatic VEGF-D concentration on OS warrants further studies on the influence of lymphangiogenesis in DLBCL on the clinical course of this disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.