Abstract
Multiple myeloma is associated with excessive tumor-induced, osteoclast-mediated bone destruction. Hypercalcemia remains the most frequent metabolic complication of myeloma in patients, and excessive osteolysis plays a major contributory role in its pathogenesis. Hypercalcemia caused by increased blood levels of PTHrP have been found in patients with solid tumors and are uncommon in patients with hematologic malignancies including multiple myeloma. Here we present a unique case of a rare variant of multiple myeloma, IgG heavy chain disease, presenting with PTHrP associated hypercalcemia.
A retrospective chart review of one patient from 2011-2013 including clinical history, laboratory data, imaging, and pathology was performed.
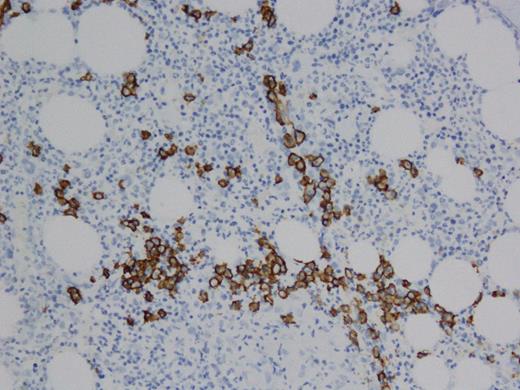
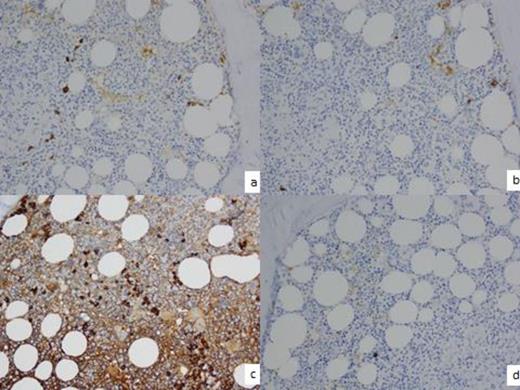
A 60 year old female with past medical history of stage IIA Hodgkin's lymphoma diagnosed in 1992, treated with total nodal radiation with recurrence in 1997 treated with 6 cycles of ABVD achieving complete remission. The patient was found to have hypercalcemia (11.0 mg/dL) and renal failure (1.29 mg/dL) in March 2011. Hypercalcemia workup revealed suppressed PTH (<3 pg/ml), elevated ionized calcium (6.1 mg/dL) elevated parathyroid related peptide (38pg/ml), normal vitamin D and ACE levels. Serum protein electrophoresis (SPEP) showed M-spike of 0.9 g/dL. Immunofixation electrophoresis (IFE) demonstrated an IgG monoclonal immunoglobulin without a corresponding light chain (figure 1). Free serum kappa and lamda light chains were within normal limits. Serum IgG was elevated (4678 mg/dL), normal IgA (127 mg/dL) and low IgM (39mg/dL). Also, Beta-2 microglobulin was elevated (14.3 mg/L). The patient was seen by hematology for monoclonal gammopathy and hypercalcemia and a solid tumor work up was recommended given that the most common the mechanism of hypercalcemia for multiple myeloma is osteoclast-driven and not PTHrP related. CT chest/abdomen/pelvis, bone scan, bone survey, mammography, pelvis ultrasound were negative. Bone marrow biopsy was performed November 2011 showing 10% plasma cells (PC) by CD138, non clonal by kappa/lambda. Patient was placed on zolendonic acid for hypercalcemia and her renal function and hypercalcemia continued to worsen over a period of months. A kidney biopsy was performed in April, 2012 and revealed acute and chronic tubulointerstitial nephritis with secondary glomerulosclerosis and mild interstitial fibrosis and tubular atrophy suggestive of sarcoidosis and the patient was placed on a course of prednisone with transient improvement in calcium and renal function. The patient presented in emergency room in April 2013 with altered mental status. She was found to have hypercalcemia (12.0 mg/dL), renal failure (1.55 mg/dL),). SPEP revealed M-spike 0.64 g/dl. IFE displayed a broad band of IgG heavy chain, without associated light chains and severe depression of the non-monoclonal IgG. Serum immunoglobulins demonstrated elevated IgG (2110 mg/dL), normal IgA (46 mg/dL) and decreased IgM (<21 mg/dL). Bone marrow biopsy showed 5% PCs (figure 2), non clonal by kappa/lambda- but exclusive for IgG by IHC, without any staining for IgA or IgM (figure 3). Cytogenetics were normal. Based on the constellation of findings and similarity to prior workup the patient was diagnosed with IgG heavy chain disease and therapy with cytoxan, dexamethasone, bortezomib was initiated. Calcium levels improved and she has recovered clinically; she is currently completing her second cycle of therapy. We plan to follow PTHrP levels along with routine paraprotein assessments.
IFE demonstrating monoclonal IgG without corresponding light chain
IFE demonstrating monoclonal IgG without corresponding light chain
CD138+ PCs
Few PCs + kappa light chain by IHC. 3b. Few PCs + for lambda light chain by IHC 3c. Majority of PCs show + IgG by IHC. 3d. PCs - IgM by IHC.
Few PCs + kappa light chain by IHC. 3b. Few PCs + for lambda light chain by IHC 3c. Majority of PCs show + IgG by IHC. 3d. PCs - IgM by IHC.
PTHrP mediated hypercalcemia is rare in patients with multiple myeloma and the main mechanism of hypercalcemia in multiple myeloma is osteoclast-mediated bone destruction. This is the first reported case of IgG heavy chain disease presenting with PTHrP related hypercalcemia. Another critical point related to this case, is that kappa/lambda staining, the primary mechanism of determining plasma cell clonality, is not useful in exclusively heavy chain disease- and can, in such cases, obscure the diagnosis of this plasma cell malignancy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.