In this issue of Blood, Chan et al have described mechanisms by which L5, the most electronegative of 5 recognized fractions of low density lipoprotein (LDL), activates both platelets and endothelium in a manner that supports thrombosis and could possibly produce ST-elevation myocardial infarctions (STEMI).1
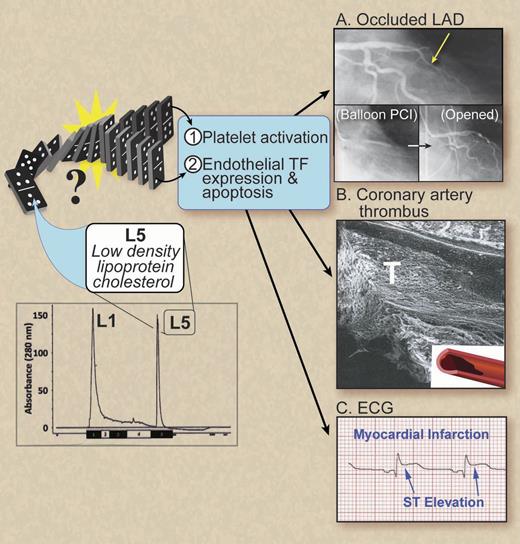
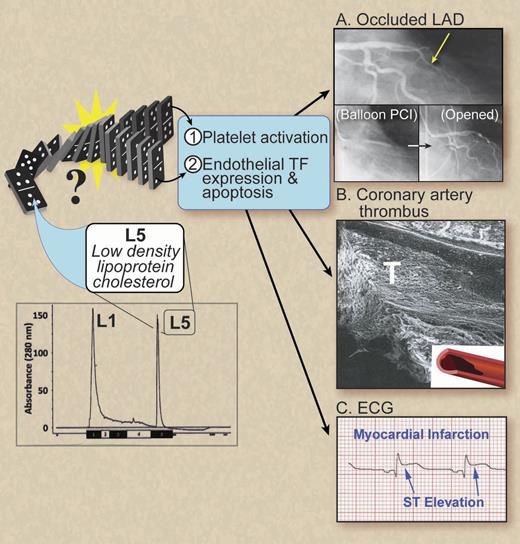
Can bad cholesterol get worse? L5, the most electronegative LDL fraction isolated chromatographically, was found to be significantly elevated in patients with STEMI compared with normal controls.1 Ex vivo, L5 not only enhanced adenosine 5′-diphosphate-stimulated platelet aggregation, platelet P-selectin expression, and GP IIb/IIIa activation but also induced both endothelial tissue factor and P-selectin expression and apoptosis. Together, these data provide mechanistic details of the thrombophilic state created by L5 that could cause a domino effect and produce an occlusive coronary artery thrombosis resulting in an STEMI. (A) Coronary angiogram showing an occluded left anterior descending coronary artery (LAD) during STEMI and inserts showing balloon percutaneous coronary intervention (PCI) and the angiogram after opening the LAD. (B) Scanning electron micrograph of bisected LAD from a pig with an occlusive thrombosis (T) causing an STEMI. (C) Electrocardiogram showing a STEMI. Professional illustration by Debra T. Dartez.
Can bad cholesterol get worse? L5, the most electronegative LDL fraction isolated chromatographically, was found to be significantly elevated in patients with STEMI compared with normal controls.1 Ex vivo, L5 not only enhanced adenosine 5′-diphosphate-stimulated platelet aggregation, platelet P-selectin expression, and GP IIb/IIIa activation but also induced both endothelial tissue factor and P-selectin expression and apoptosis. Together, these data provide mechanistic details of the thrombophilic state created by L5 that could cause a domino effect and produce an occlusive coronary artery thrombosis resulting in an STEMI. (A) Coronary angiogram showing an occluded left anterior descending coronary artery (LAD) during STEMI and inserts showing balloon percutaneous coronary intervention (PCI) and the angiogram after opening the LAD. (B) Scanning electron micrograph of bisected LAD from a pig with an occlusive thrombosis (T) causing an STEMI. (C) Electrocardiogram showing a STEMI. Professional illustration by Debra T. Dartez.
Most importantly, L5 was significantly elevated in STEMI patients when compared with otherwise healthy control subjects. These changes in the fractional composition of LDL, often called “bad cholesterol” because of its role in atherogenesis, may add thrombophilic properties. Platelets that were exposed to clinically relevant doses of purified L5 exhibited enhanced adenosine 5′-diphosphate-stimulated aggregation, P-selectin expression, and GP IIb/IIIa activation with signaling through platelet-activating factor receptor and lectin-like oxidized LDL receptor-1. Endothelium exposed to L5 in a likewise manner expressed tissue factor and P-selectin that also supported platelet activation and aggregation. As previously shown, L5 also mediated endothelial apoptosis by reducing expression of the fibroblast growth factor-2 (FGF2) promoter via an epigenetic mechanism (CpG methylation). Injecting L5 into mice corroborated these ex vivo findings. Does elevated L5 cause a domino effect that is sufficient to activate platelets and endothelium, induce endothelial apoptosis, and produce occlusive coronary artery thrombosis and STEMI (see figure)?
The history of establishing occlusive coronary artery thrombosis as the cause of STEMI has become an object lesson in investigative pathology and clinical trials. Between William Heberden’s original description of angina in 17722 and the 1970s, the wide range of coronary thrombi found at autopsy of patients dying of suspected heart disease generated considerable debate as to its causative role. It was not until the pioneering work of DeWood,3 Rentrop,4 and several outstanding pathologists5 in the 1970s that occlusive coronary artery thrombosis became accepted as the leading cause of STEMI. The key steps in resolving this debate were refinement in methods of detecting coronary thromboses, recognition that clot lysis occurs over time, and identification of coronary plaques that were vulnerable to rupture. A vulnerable plaque is characterized in part by a thin fibrous cap, high lipid content, inflammatory mediators, and extensive adventitial and intimal neovascularity. When vulnerable plaques rupture and expose subendothelium and plaque contents to flowing blood, coronary artery thrombosis develops and, if occlusive, can result in a STEMI. It is equally important to note that a subtler finding of plaque erosion is nonetheless also associated with coronary artery thrombosis.6,7
Identification of the precise mechanism(s) that causes vulnerable plaques to rupture or the sequence of events that precipitate coronary artery thrombosis and STEMI has been elusive. In a meta-regression analysis that included 36 studies to compute the population-attributable fraction, ie, cases that could be avoided if a risk factor were removed, the following hierarchy of suspected stimuli of myocardial infarction was established: air pollution, physical exertion, alcohol, coffee, negative emotions, anger, heavy meal, positive emotions, sexual activity, cocaine use, marijuana smoking, and respiratory infections.8 The relatively low frequency of STEMI with each of these stimuli, however, suggests that other factors or cofactors are likely to be involved. Especially relevant to this argument is the consistent finding that small, “non-culprit” coronary plaques appear, over time, to be responsible for as many coronary events as larger “culprit lesions.”9,10 In contrast, the biological properties of L5 could produce STEMI by several mechanisms: first, initiating plaque erosion or rupture by supporting endothelial apoptosis and second, mediating coronary thrombogenesis via platelet and endothelial activation.
There are limitations to this study. A total of 30 patients is small for a STEMI study, but larger studies are underway that will address the somewhat wide variation in L5 levels in the patients included in this study. At present, the mechanism by which L5 becomes elevated in plasma is unknown as is the duration of elevation prior to STEMI. Such information would be important to propose therapeutic approaches to reduce L5 levels or modify it to be less thrombogenic. The association of elevated L5 levels with other traditional risk factors such as hyperlipidemia and diabetes suggests that risk factor reduction may be a first step. Likewise, low dose aspirin was shown to blunt L5-mediated endothelial apoptosis in vitro and it will be important to determine if this biological effect is also operative in vivo. The exact constituent of L5 that confers the described biological properties has not been defined yet. Also, it is not clear if L5 is present in other populations beyond those reported or how gender or menopausal status might influence L5 levels. The procedures required for measuring L5 are rigorous and may limit its translation to general usage unless simpler methods can be developed. All of these limitations are surmountable.
Definitive proof of a single mechanism mediating coronary artery thrombosis and STEMI seems unlikely to be forthcoming given the pleomorphic nature of atherosclerotic plaques and the myriad of potential interactions with the cellular and humoral thrombosis pathways. Consideration will need to be given to whether suspected stimuli are additive or synergistic, if there is a hierarchy among them, or if other cofactors are involved. The data presented by Chan et al1 clearly document that elevations in L5 could initiate a domino effect that produces an occlusive coronary artery thrombosis and STEMI.
Conflict-of-interest disclosure: The author declares no competing financial interests.