Key Points
Allogeneic-donor–derived cells can be genetically modified to eliminate expression of HLA-A.
HLA-A disruption from donor cells is a step toward generating allogeneic cells as an off-the-shelf therapeutic.
Abstract
Long-term engraftment of allogeneic cells necessitates eluding immune-mediated rejection, which is currently achieved by matching for human leukocyte antigen (HLA) expression, immunosuppression, and/or delivery of donor-derived cells to sanctuary sites. Genetic engineering provides an alternative approach to avoid clearance of cells that are recognized as “non-self” by the recipient. To this end, we developed designer zinc finger nucleases and employed a “hit-and-run” approach to genetic editing for selective elimination of HLA expression. Electro-transfer of mRNA species coding for these engineered nucleases completely disrupted expression of HLA-A on human T cells, including CD19-specific T cells. The HLA-Aneg T-cell pools can be enriched and evade lysis by HLA-restricted cytotoxic T-cell clones. Recognition by natural killer cells of cells that had lost HLA expression was circumvented by enforced expression of nonclassical HLA molecules. Furthermore, we demonstrate that zinc finger nucleases can eliminate HLA-A expression from embryonic stem cells, which broadens the applicability of this strategy beyond infusing HLA-disparate immune cells. These findings establish that clinically appealing cell types derived from donors with disparate HLA expression can be genetically edited to evade an immune response and provide a foundation whereby cells from a single donor can be administered to multiple recipients.
Introduction
Ex vivo manipulation of autologous cell products that are then returned to the patient can restore cellular functions in individuals with incurable diseases.1-5 However, this manufacturing of recipient-specific clinical-grade products is time-consuming and labor-intensive, as well as expensive, and the desired cells are often unavailable when required for many patients. Engraftment of donor-derived (allogeneic) cells to reconstitute cellular functions is advantageous compared with infusing patient-derived cells, as the ability to manufacture and validate therapeutic and fully functional cell preparations in advance improves safety, consistency, and availability. Survival of an allograft bearing disparate human leukocyte antigens (HLAs) in an immunocompetent recipient depends on avoiding or overcoming an immune response to the infused cells. Rejection is primarily mediated by host-derived T cells recognizing nonself major and/or minor histocompatibility antigens (mHAgs). Therefore, the most effective approach to sustaining allograft survival is to preclude mismatches between the donor and recipient HLA, as highlighted by the improved survival of HLA-matched grafts after allogeneic hematopoietic stem cell6 and solid organ transplantation.7 This led us to investigate whether an immune response could be avoided by eliminating expression of 1 or more mismatched HLAs on donor-derived cells.
Some viral proteins inhibit HLA folding and surface display, which allows infected cells to escape T-cell recognition,8 and enforced expression of these viral-derived transgenes can downregulate HLA expression.9 As an alternative, the Cre-LoxP system can be deployed to disrupt the β2-microglobulin locus, and thus HLA class I expression, but this requires removal of antibiotic-resistant genes by Cre recombinase, which may introduce unwanted recombination events.10 We and others have previously attempted to downregulate HLA class I expression by introducing small interfering RNA targeting HLA heavy chains or β2-microglobulin.11-13 Although these posttranscriptional approaches reduce antigen levels, they require sustained transgene expression and, moreover, reduce but do not completely eliminate HLA expression. Given that an αβ T-cell receptor (TCR) response can be triggered by just a small number of cell-surface HLA molecules,14 we sought an alternative to achieve complete elimination of HLA. Here we show that transient expression of zinc finger nucleases (ZFNs)15 targeting the HLA-A locus can permanently and completely eliminate HLA-A expression from (1) a model cell line, (2) primary and genetically modified human T cells used in clinical trials, and (3) human embryonic stem cells (hESCs). These results highlight a path toward rapid human application, as circulating natural killer (NK) cells could be prevented from recognizing cells engineered to lose HLA expression.
Materials and methods
Study approval
Peripheral blood mononuclear cells (PBMCs) were obtained from healthy adult volunteer donors who had provided informed consent from Gulf Coast Regional Center (Houston, TX) in accordance with the Declaration of Helsinki, and who participated in research approved by the institutional review board of The University of Texas MD Anderson Cancer Center.
Design of ZFNs targeting HLA-A
ZFNs containing 5 or 6 fingers were designed and assembled using an established archive of prevalidated 2-finger and 1-finger modules essentially as described.16 Briefly, the coding sequence of HLA-A was scanned for locations at which 2 such ZFNs (designated as ZFN-L and ZFN-R) could be targeted to sites that were separated by 5 base pairs and located on opposite DNA strands. The nucleotide targets for candidate ZFN pairs were then checked for divergence from other HLA coding sequences. Genes encoding the ZFN designs were assembled using a polymerase chain reaction (PCR)-based procedure and cloned into a plasmid.
Cell culture
HEK293 cells were maintained in Dulbecco’s modified Eagle medium (DMEM; Lonza, Basel, Switzerland) supplemented with 10% heat-inactivated fetal bovine serum (FBS; Lonza) and 2 mmol/L l-glutamine (Invitrogen, Carlsbad, CA). Epstein-Barr-virus–transformed lymphoblastoid cell line (EBV-LCL), 721.221, EL-4, NALM-6, and Daudi cell lines were maintained in RPMI 1640 (Lonza) supplemented with 10% FBS and 2 mmol/L l-glutamine (designated as complete medium). The identity of these cell lines was confirmed by short tandem repeat DNA fingerprinting. CD8+ cytotoxic T-lymphocyte (CTL) clones specific for mHAgs were HLA-A*03:01-restricted 7A7 recognizing peptide RVWDLPGVLK encoded by PANE1 transcripts and HLA-A*02:01-restricted GAS2B3-5 recognizing CIPPDSLLFPA peptide from ORF +2/48 in C19ORF48. CTLs were thawed 1 day before the assay and maintained in RPMI 1640 supplemented with 10% human albumin serum, 2 mmol/L l-glutamine, 20 ng/mL interleukin 15 (IL-15; PeproTech, Rocky Hill, NJ), and 20 IU/mL IL-2 (Chiron, Emeryville, CA).
Activation of primary T cells from PBMCs
T cells were activated in vitro by stimulating PBMCs with OKT3 (eBioscience, San Diego, CA) preloaded onto artificial antigen presenting cells (aAPCs; clone 4: K562 cells genetically modified to stably coexpress CD19, CD64, CD86, CD137L, and a membrane-bound mutein of interleukin [IL-15] synchronously expressed with enhanced green fluorescence protein17,18 ) at a ratio of 1:1 (T cells: γ-irradiated [100Gy] aAPC) in complete media supplemented with 50 IU/mL IL-2 (added every other day). OKT3-loaded aAPC were re-added every 14 days to sustain T-cell proliferation.
Generation of CD19-specific CAR+T cells
Our approach to manufacturing clinical-grade chimeric antigen receptor–positive (CAR+)T cells was adapted to generate CD19-specific T cells.19 DNA plasmids coding for Sleeping Beauty (SB) transposon CD19RCD28 and SB hyperactive transposase SB11 were simultaneously electro-transferred (Human T-Cell Nucleofector solution, program U-014), using a Nucleofector II device (Lonza), into T cells derived from PBMCs. A population of CAR+T cells was selectively numerically expanded by adding on the day of electroporation and re-adding every 14 days (at a 1:2, T cell:aAPC ratio) γ-irradiated (100 Gy) aAPC (clone 4 without OKT3 loading) in the presence of 50 IU/mL IL-2 (added every other day).
In vitro transcription of messenger RNA
In vitro–transcribed mRNA species were prepared as previously described.20 In brief, the DNA template plasmids coding for ZFN-L and ZFN-R (supplemental Figure 1) were linearized with XhoI. After in vitro transcription (RiboMAX Large Scale RNA Production System-T7; Promega, Madison, WI) and capping (ARCA cap analog; Ambion, Austin, TX) according to manufacturers’ instructions, poly-adenines were added using the poly A tailing kit (Ambion). The integrity of the mRNA species was validated on a denaturing 1% agarose gel with 3-(N-morpholino) propanesulphonic acid buffer, and concentration was determined by spectrophotometer (BioRad, Hercules, CA) at OD260. The mRNA was vialed and stored at −80°C for one-time use.
Electro-transfer of ZFNs
For the modification of HEK293, expression vectors encoding HLA-A targeting ZFNs (supplemental Figure 1) were introduced by Nucleofection (Lonza) according to the manufacturer’s protocol and described elsewhere.20 After electroporation, cells were immediately placed in prewarmed complete media and cultured at 37°C and 5% CO2 for 4-6 hours, at which point 50 IU/mL IL-2 was added for further culture. In “cold shock” experiments,21 after overnight culture in a 37°C–5% CO2 incubator, T cells were transferred to a 30°C–5% CO2 incubator and cultured for 3 days before being returned to a 37°C–5% CO2 incubator before analysis.
Enrichment of HLA-Aneg cells
After washing cells with phosphate-buffered saline supplemented with 2% FBS and 2 mM EDTA, cells were labeled with phycoerythrin (PE) anti-HLA-A2 (BD Biosciences, San Jose, CA) at 4°C for 15 minutes, washed, and labeled with anti-PE microbeads (Miltenyi Biotec, Auburn, CA) for 10 minutes. After washing, labeled cells were passed through an LD Column (Miltenyi Biotec), and the flow-through fraction was collected and cultured. T cells were propagated on γ-irradiated OKT3-loaded aAPC, and CAR+T cells were propagated on CD19+aAPC (not OKT3-loaded) in complete media supplemented with 50 IU/mL IL-2 (added every other day).
Flow cytometry
The following antibodies were used: PE-conjugated antibodies; anti-HLA-A2 (clone BB7.2), anti-CD56 (clone B159), anti-HLA-DR (clone G46-6), mouse IgG2bκ, mouse IgG2aκ, FITC conjugated antibodies; anti-CD4 (clone RPA-T4), anti-CD8 (clone HIT8a), nonspecific mouse IgG1, PE and APC anti-CD3 (clone SK7), secondary reagent streptavidin-PE (all from BD Biosciences), biotin-conjugated anti-HLA-A3 (clone 4i153), APC anti-HLA-G (clone MEMG19), PE anti-HLA class I (clone W6/32; Abcam, Cambridge, MA), and PE anti-HLA-E (clone 3D12; Biolegend, San Diego, CA). The Alexa 488-conjugated anti-CD19RCD28 CAR antibody was generated in our laboratory. We added propidium iodide (Sigma-Aldrich) to exclude dead cells from analysis. Data were acquired on a FACS Calibur using CellQuest version 3.3 (BD Biosciences) and analyzed by FlowJo version 7.6.1 (Tree Star Inc., Ashland, OR).
Surveyor nuclease assay
The level of modification of the HLA-A gene sequence in ZFN-transfected cells was determined by the Surveyor nuclease assay.22 In brief, genomic DNA from ZFN-modified cells underwent PCR with oligonucleotide primers designed to amplify the ZFN target regions within HLA-A2 and HLA-A3 genetic loci. After denaturing and re-annealing, Surveyor endonuclease (Transgenomic, Omaha, NE) was used to cut heteroduplex DNA products that were resolved by polyacrylamide gel electrophoresis. Percentage target modification was quantified by densitometry. The PCR primers used for the amplification of target loci were HLA-A3 forward, 5′-GGGGCCGGAGTATTGGGACCA-3′; HLA-A3 reverse, 5′-CCGTCGTAGGCGTCCTGCCG-3′; HLA-A2 forward, 5′-GGGTCCGGAGTATTGGGACGG-3′; and HLA-A2 reverse; 5′-TTGCCGTCGTAGGCGTACTGGTG-3′.
51Chromium release assay
Target cells were labeled with 0.1 mCi 51Cr for 2 hours. After washing 3 times with ice-cold complete media, labeled cells were diluted and distributed at 103 target cells in 100 μL per well in 96-well, v-bottomed plates. In the peptide titration assay, target cells were incubated with 10-fold serial dilutions of the peptides for 30 minutes at room temperature. CTLs were added at indicated effector-to-target ratios. After a 4- to 6-hour incubation at 37°C in 5% CO2, 50 μL of cell-free supernatants were collected and counted on a TopCount device (Perkin Elmer, Shelton, CT). All assays were performed in triplicate. In some assays, parental HEK293 and HLA-A modified HEK293 clones were treated with 600 IU/mL interferon γ (IFN-γ; R&D systems, Minneapolis, MN) and 10 ng/mL tissue necrosis factor-α (TNF-α; R&D systems) for 48 hours before assay. The percentage specific lysis was calculated as follows: ([experimental cpm − spontaneous cpm]/[maximum cpm − spontaneous cpm]) × 100.
Culture and differentiation of hESCs
The hESC line WIBR3 (Whitehead Institute Center for Human Stem Cell Research, Cambridge, MA)23 was maintained, as described previously,24 on mitomycin C–inactivated mouse embryonic fibroblast feeder layers in hESC medium (DMEM/F12 [Invitrogen] supplemented with 15% FBS, 5% KnockOut Serum Replacement [Invitrogen], 1 mM glutamine [Invitrogen], 1% nonessential amino acids [Invitrogen], 0.1 mM β-mercaptoethanol [Sigma, St. Louis, MO], and 4 ng/mL FGF2 [R&D systems]). Targeted hESCs were differentiated into fibroblast-like cells as described previously.25 Briefly, differentiation was induced by embryoid body (EB) formation in nonadherent suspension culture dishes (Corning, Corning, NY) in DMEM medium supplemented with 15% FBS for 5 days. EBs were subsequently plated onto adherent tissue culture dishes and passaged according to primary fibroblast protocols, using trypsin for at least 4 passages before the start of experiments.
ZFN-mediated genome editing of hESCs
hESCs were cultured in ρ-associated protein kinase inhibitor (Stemolecule; Stemgent, Cambridge, MA) 24 hours before electroporation. Cells were harvested using 0.05% trypsin/EDTA solution (Invitrogen) and resuspended in phosphate-buffered saline. Ten million cells were electroporated (Gene PulserXcell System, Bio-Rad: 250 V, 500 µF, 0.4 cm cuvettes) with 35 µg donor plasmid encoding the puromycin-resistant gene under the control of phosphoglycerate kinase promoter flanked by 5′ and 3′ groups homologous to the putative ZFN binding region of HLA-A24 and 7.5 µg of each ZFN-encoding plasmid, or 35 µg of donor plasmid and 10 µg of each ZFN-encoding mRNA. Cells were subsequently plated on DR4 mouse embryonic fibroblast feeder layers in hESC medium supplemented with ρ-associated protein kinase inhibitor for the first 24 hours. Puromycin selection (0.5 µg/mL) was initiated 72 hours after electroporation. Individual puromycin-resistant colonies were picked and expanded 10 to 14 days after electroporation. Correct targeting and gene disruption was verified by Southern blot analysis and sequencing of the genomic locus.
Results
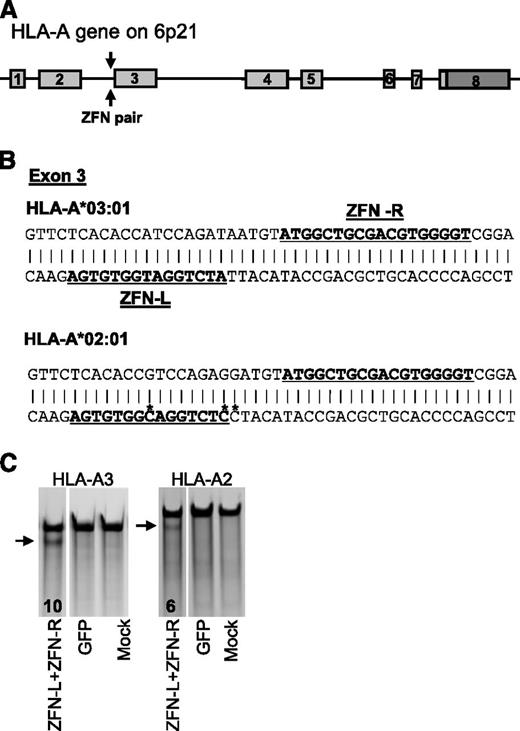
Design and Validation of ZFNs
ZFNs were designed to cleave a predefined site within the genomic coding sequence of the endogenous human HLA-A genes (Figure 1A-B). Expression of these artificial nucleases in human cells should eliminate expression of HLA-A molecules via error-prone repair of introduced double-strand breaks leading to disruption of the reading frame. To evaluate the ability of these ZFNs to disrupt HLA-A expression, we initially used the HEK293 cell line, which coexpresses HLA-A*03:01 (HLA-A3) and HLA-A*02:01 (HLA-A2). After transfecting HEK293 cells with expression plasmids encoding the ZFNs, we used allele-specific PCR and the Surveyor nuclease assay22 to quantify the level of gene modification at the anticipated ZFN target sites. These data demonstrated ∼10% modification of HLA-A3 and ∼6% modification of HLA-A2, using this ZFN pair (Figure 1C).
Designed ZFNs disrupt HLA-A expression on HEK293. (A) Schematic of the HLA-A genetic loci. Arrows indicate the location of the putative ZFN binding sites. (B) ZFN binding sites within the HLA-A alleles expressed by HEK293. A 46-base pair segment of the HLA-A*03:01 and HLA-A*02:01 alleles is shown, with bold and underlined nucleotides highlighting the anticipated binding sites for the ZFN-L and ZFN-R monomers, respectively. Cleavage occurs in the region between these sites. Note that HLA-A*02:01 differs from and HLA-A*03:01 at 3 positions within this region, which are marked with an asterisk. ZFN-L was designed to ignore these polymorphisms and to cleave both alleles. (C) Levels of HLA-A3 and HLA-A2 genetic disruption assessed by the Surveyor nuclease assay. The lower (fast-moving) bands (arrows) are digestion products indicating ZFN-mediated gene modification. The numbers indicate the percentage of modified HLA-A alleles based on densitometry. GFP represents genetically modified HEK293 expressing GFP as a control. Mock represents no DNA used.
Designed ZFNs disrupt HLA-A expression on HEK293. (A) Schematic of the HLA-A genetic loci. Arrows indicate the location of the putative ZFN binding sites. (B) ZFN binding sites within the HLA-A alleles expressed by HEK293. A 46-base pair segment of the HLA-A*03:01 and HLA-A*02:01 alleles is shown, with bold and underlined nucleotides highlighting the anticipated binding sites for the ZFN-L and ZFN-R monomers, respectively. Cleavage occurs in the region between these sites. Note that HLA-A*02:01 differs from and HLA-A*03:01 at 3 positions within this region, which are marked with an asterisk. ZFN-L was designed to ignore these polymorphisms and to cleave both alleles. (C) Levels of HLA-A3 and HLA-A2 genetic disruption assessed by the Surveyor nuclease assay. The lower (fast-moving) bands (arrows) are digestion products indicating ZFN-mediated gene modification. The numbers indicate the percentage of modified HLA-A alleles based on densitometry. GFP represents genetically modified HEK293 expressing GFP as a control. Mock represents no DNA used.
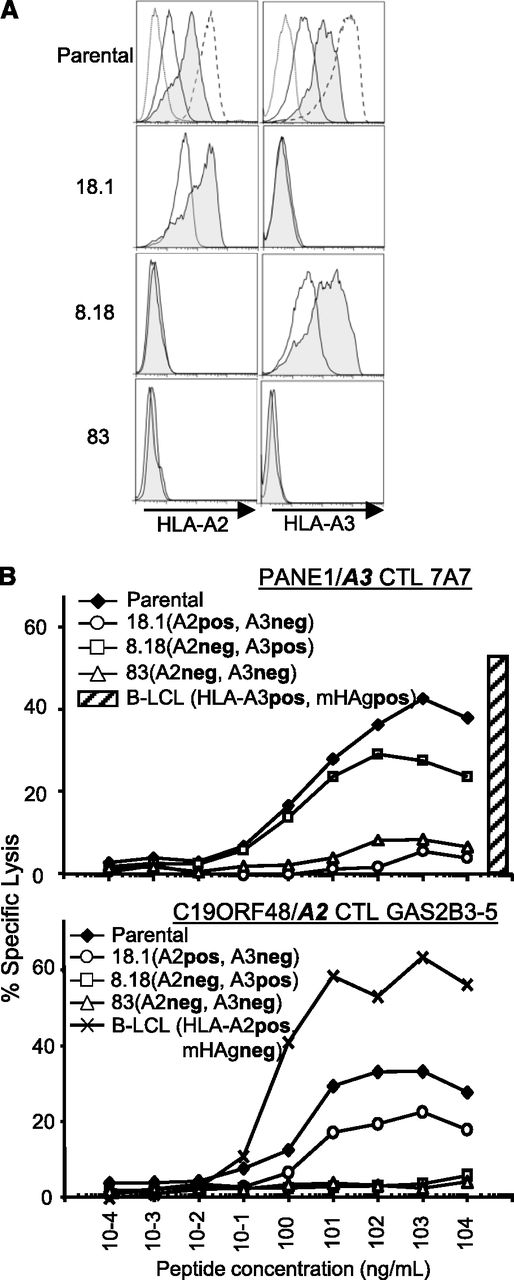
Isolation and functional validation of HLA-Aneg HEK293
We used limiting dilution to obtain single-cell clones from the ZFN-modified HEK293 pool to assess the effect of disrupting HLA-A expression. Sequencing revealed clones that carried insertions or deletions (indels) within the expected ZFN-binding sites in HLA-A2, HLA-A3, or both alleles (supplemental Figure 2), which resulted in a frame shift leading to premature termination of translation. Because the steady-state level of HLA-A expression in HEK293 is low compared with hematopoietic cells, such as an EBV-LCL, we exposed the HEK293 cells to pro-inflammatory cytokines known to augment HLA levels.26 The addition of IFN-γ and TNF-α increased expression of both HLA-A alleles in parental HEK293 cells (Figure 2A, top). In contrast, ZFN-treated single-cell–derived HEK293 clones harboring mutations in HLA-A2 and/or HLA-A3 did not express these proteins even after induction by IFN-γ and TNF-α (Figure 2A, bottom 3 panels). Next, we asked whether the loss of HLA-A expression on the ZFN-modified clones would preclude T-cell recognition by challenging with HLA-A3- and HLA-A2-restricted CTLs. As expected, an HLA-A3-restricted CTL clone 7A7 demonstrated robust specific lysis of the HLA-A3+ parental HEK293 line loaded with a serial dilution of the cognate peptide (Figure 2B, top). Clone 8.18 that had lost expression of HLA-A2 allele, but is wild-type at HLA-A3, was also lysed by this HLA-A3-restricted CTL. In contrast, when pulsed with the same peptide, clones 18.1 and 83, which had been edited to eliminate HLA-A3 expression, were not lysed by the HLA-A3-restricted CTL clone 7A7 (Figure 2B, top). We also evaluated the cytolytic activity of an HLA-A2-restricted CTL clone GAS2B3-5 and observed robust killing activity when presented with the parental HEK293 or the HLA-A2 wild-type clone 18.1, whereas the ZFN-modified HLA-A2neg clone 8.18 and the HLA-A2/A3 double-knock out clone 83 were spared from lysis (Figure 2B, bottom). These data demonstrate that treatment with ZFNs completely eliminates HLA-A expression, resulting in protection from HLA-A restricted CTL-mediated killing, even under proinflammatory conditions known to upregulate endogenous HLA-A expression.
Isolation of HLA-AnegHEK293. (A) Loss of HLA-A2 and HLA-A3 protein expression. Flow cytometry analysis of HLA-A2 and HLA-A3 expression on parental HEK293 and 3 derived genetically modified clones with loss of HLA-A (numbered 18.1, 8.18, and 83). Dotted lines represent isotype (HLA-A2) or SA-PE (HLA-A3) controls; solid line represents HLA-A expression without IFN-γ and TNF-α, and filled lines represent HLA-A expression after culturing with 600 IU/mL IFN-γ and 10 ng/mL TNF-α for 48 hours. Dashed lines in the parental column represent HLA-A2 or HLA-A3 expression on EBV-LCL. (B) Resistance to CTL-mediated lysis. Parental HEK293 and derived HLA-Aneg clones were cultured with IFN-γ and TNF-α for 48 hours and pulsed with serial dilutions of the cognate HLA-A3 peptide RVWDLPGVLK (derived from PANE1 and recognized by CTL clone 7A7)27 or the HLA-A2 peptide CIPPDSLLFPA (derived from C19ORF48/A2 and recognized by CTL clone GAS2B3-5)28 and evaluated for recognition by CTL clones in a 4-hour 51Cr release assay at an effector-to-target ratio of 20:1.HLA-A2+ LCL (hatched bar) that expresses PANE1mHAg (not peptide-loaded) were used as a positive control.
Isolation of HLA-AnegHEK293. (A) Loss of HLA-A2 and HLA-A3 protein expression. Flow cytometry analysis of HLA-A2 and HLA-A3 expression on parental HEK293 and 3 derived genetically modified clones with loss of HLA-A (numbered 18.1, 8.18, and 83). Dotted lines represent isotype (HLA-A2) or SA-PE (HLA-A3) controls; solid line represents HLA-A expression without IFN-γ and TNF-α, and filled lines represent HLA-A expression after culturing with 600 IU/mL IFN-γ and 10 ng/mL TNF-α for 48 hours. Dashed lines in the parental column represent HLA-A2 or HLA-A3 expression on EBV-LCL. (B) Resistance to CTL-mediated lysis. Parental HEK293 and derived HLA-Aneg clones were cultured with IFN-γ and TNF-α for 48 hours and pulsed with serial dilutions of the cognate HLA-A3 peptide RVWDLPGVLK (derived from PANE1 and recognized by CTL clone 7A7)27 or the HLA-A2 peptide CIPPDSLLFPA (derived from C19ORF48/A2 and recognized by CTL clone GAS2B3-5)28 and evaluated for recognition by CTL clones in a 4-hour 51Cr release assay at an effector-to-target ratio of 20:1.HLA-A2+ LCL (hatched bar) that expresses PANE1mHAg (not peptide-loaded) were used as a positive control.
Disruption of HLA-A in primary T cells
To extend our results to clinically relevant primary cells, we evaluated the activity of the HLA-A-specific ZFNs in human T cells. Because ZFNs require only short-term expression to achieve stable disruption of desired target genes, we transiently expressed ZFNs from an in vitro–transcribed mRNA. Electro-transfer of mRNA encoding the ZFNs into T cells from an HLA-A2 homozygous donor (HLA-A2 being the most common HLA-A allele in whites29 ) rendered ∼19% of these T cells HLA-A2-negative (Figure 3A, top). We have previously demonstrated that transiently lowering the incubation temperature after transfection can increase ZFN activity.20,21 Subjecting electroporated T cells to a transient hypothermia21 elevated the proportion of HLA-A2neg cells to up to 57% in an mRNA dose-dependent manner (Figure 3A, bottom). Functional elimination of HLA-A2 was further confirmed by probing HLA-A2-transduced 721.221 cells with a pan class I antibody (supplemental Figure 3).
Loss of HLA-A expression on primary OKT3-propagated T cells after genetic editing with ZFNs. (A). Loss of cell surface expression of HLA-A2 after electro-transfer of mRNA species encoding ZFN-L and ZFN-R targeting HLA-A2 (top). T cells were harvested 6 days after initial stimulation with γ-irradiated aAPC. Five million T cells were premixed with ZFN mRNA in 100 μL Human T-cell Nucleofector solution and electroporated in a cuvette using a Nucleofector II device with program T-20. Coexpressions of HLA-A2, CD4, and CD8 were analyzed 4 days after electro-transfer of graded doses of the mRNA species encoding ZFN-L and ZFN-R. Flow cytometry data were gated on the propidium iodide-negative, live cell population. Numbers in the lower-right quadrant indicate the percentage of CD4 and CD8+ T cells that are HLA-Aneg. Improved disruption of HLA-A expression by cold shock (bottom). Data were collected 4 days after electro-transfer of graded doses of the mRNA species encoding ZFN-L and ZFN-R. Cells were cultured at 30°C from days 1 to 3 after electro-transfer of ZFNs, returned to 37°C, and cultured for 1 additional day before analysis. (B) Improved efficiency of HLA-A disruption by ZFN-L and ZFN-R fused to the heterodimeric FokI domain variants. mRNA species encoding the ZFN-L and ZFN-R heterodimeric FokI mutants EL:KK targeting HLA-A were electro-transferred into primary T cells. HLA-A2 expression was analyzed after culturing the cells for 4 days at 37°C or 3 days at 30°C followed by 37°C for 1 day. X-axis represents CD4 and CD8 expression and y-axis represents HLA-A2 expression.
Loss of HLA-A expression on primary OKT3-propagated T cells after genetic editing with ZFNs. (A). Loss of cell surface expression of HLA-A2 after electro-transfer of mRNA species encoding ZFN-L and ZFN-R targeting HLA-A2 (top). T cells were harvested 6 days after initial stimulation with γ-irradiated aAPC. Five million T cells were premixed with ZFN mRNA in 100 μL Human T-cell Nucleofector solution and electroporated in a cuvette using a Nucleofector II device with program T-20. Coexpressions of HLA-A2, CD4, and CD8 were analyzed 4 days after electro-transfer of graded doses of the mRNA species encoding ZFN-L and ZFN-R. Flow cytometry data were gated on the propidium iodide-negative, live cell population. Numbers in the lower-right quadrant indicate the percentage of CD4 and CD8+ T cells that are HLA-Aneg. Improved disruption of HLA-A expression by cold shock (bottom). Data were collected 4 days after electro-transfer of graded doses of the mRNA species encoding ZFN-L and ZFN-R. Cells were cultured at 30°C from days 1 to 3 after electro-transfer of ZFNs, returned to 37°C, and cultured for 1 additional day before analysis. (B) Improved efficiency of HLA-A disruption by ZFN-L and ZFN-R fused to the heterodimeric FokI domain variants. mRNA species encoding the ZFN-L and ZFN-R heterodimeric FokI mutants EL:KK targeting HLA-A were electro-transferred into primary T cells. HLA-A2 expression was analyzed after culturing the cells for 4 days at 37°C or 3 days at 30°C followed by 37°C for 1 day. X-axis represents CD4 and CD8 expression and y-axis represents HLA-A2 expression.
Achieving a clinically relevant level of HLA-A disruption in primary T cells
With a view to the clinical application of the HLA-targeted ZFNs, we evaluated the use of the “high-fidelity” obligate heterodimeric FokI domains EL:KK, which are designed to decrease potential off-target cleavage events by preventing homodimerization.30 Use of mRNA encoding the EL:KK ZFN variants of ZFN-L and ZFN-R resulted in a marked increase in HLA-Aneg T cells, eliminating HLA-A expression in up to 52% of the T-cell population, despite limiting doses of mRNA (2.5 µg each ZFN; Figure 3B). A single round of HLA-A-positive T-cell depletion with antibody-coated paramagnetic beads readily increased the HLA-A2neg T-cell fraction to more than 95% of the population without affecting CD4 or CD8 expression (Figure 4A). Analysis of this HLA-A2neg population by the Surveyor nuclease assay (Figure 4B) and direct DNA sequencing (Figure 4C) revealed nearly 100% editing of the HLA-A2 alleles precisely within the region targeted by the ZFNs. Together, these data demonstrate that ZFN-driven genome editing can rapidly generate an HLA-Aneg T-cell population.
Enrichment of HLA-Aneg primary T cells after genetic editing with ZFNs. (A) Generation of an HLA-A2neg T-cell population. HLA-A2neg T cells were enriched by magnetic bead-based selection. Input dose of mRNA coding for ZFN and 3-day culture conditions (37°C vs 30°C) after electro-transfer of mRNA are indicated. The numbers represent HLA-A2 negative population within the CD4- and CD8-positive population. EL:KK, obligate heterodimer mutant FokI cleavage domain; wt, wild type FokI cleavage domain. (B) Surveyor nuclease assay of the enriched HLA-A2neg T cells. Analysis of T cells enriched for loss of HLA-A2 expression demonstrates disruption in the HLA-A2 locus by the appearance of a fast-moving band (arrow). (C) Sequencing of the HLAneg T cells. PCR products using HLA-A2-specific primers from enriched cell (2.5 μg ZFNs, EL:KK FokI domain, 30°C treatment) were cloned into a TOPO vector (Invitrogen), and plasmid products were sequenced. The wild-type sequence is listed at the top, with the expected ZFN binding sites underlined. Shown below are the sequences obtained from the ZFN-treated and enriched cells. Deletions are indicated by hyphens, and sequence changes are highlighted in bold. All 18 sequence changes result in frame shifts predicted to prevent protein translation.
Enrichment of HLA-Aneg primary T cells after genetic editing with ZFNs. (A) Generation of an HLA-A2neg T-cell population. HLA-A2neg T cells were enriched by magnetic bead-based selection. Input dose of mRNA coding for ZFN and 3-day culture conditions (37°C vs 30°C) after electro-transfer of mRNA are indicated. The numbers represent HLA-A2 negative population within the CD4- and CD8-positive population. EL:KK, obligate heterodimer mutant FokI cleavage domain; wt, wild type FokI cleavage domain. (B) Surveyor nuclease assay of the enriched HLA-A2neg T cells. Analysis of T cells enriched for loss of HLA-A2 expression demonstrates disruption in the HLA-A2 locus by the appearance of a fast-moving band (arrow). (C) Sequencing of the HLAneg T cells. PCR products using HLA-A2-specific primers from enriched cell (2.5 μg ZFNs, EL:KK FokI domain, 30°C treatment) were cloned into a TOPO vector (Invitrogen), and plasmid products were sequenced. The wild-type sequence is listed at the top, with the expected ZFN binding sites underlined. Shown below are the sequences obtained from the ZFN-treated and enriched cells. Deletions are indicated by hyphens, and sequence changes are highlighted in bold. All 18 sequence changes result in frame shifts predicted to prevent protein translation.
Disruption of HLA-A in T cells genetically modified to redirect specificity
To demonstrate the potential utility of HLA editing, we next focused on a specific class of cells that could be broadly used in allogeneic settings after elimination of HLA expression: cytotoxic T cells genetically modified to express a universal CAR to redirect specificity toward tumor-associated antigens independent of HLA recognition.31 Indeed, we and others are currently infusing patient-specific CAR+T cells for the investigational treatment of CD19+ malignancies.2,3,31-35 Recently, we have published results indicating that CAR+T cells retain redirected specificity for CD19 when ZFNs are used to eliminate endogenous αβTCR expression.20 Such TCR-edited T cells demonstrate both improved potency and safety (amelioration of graft-versus-host disease) in vivo.36 To further explore the potential of “off-the-shelf” T-cell therapies, we investigated whether ZFNs could eliminate HLA-A expression in CD19-specific CAR+T cells. PBMCs genetically modified by synchronous electro-transfer of DNA plasmids derived from the SB transposon/transposase system followed by selective propagation on CD19+ aAPC37 resulted in expression of the CD19-specific CAR (designated CD19RCD28) in more than 90% of the T cells. These SB and aAPC platforms have been adapted for human application in 4 clinical trials (Clinicaltrials.gov trials NCT01497184, NCT01362452, NCT00968760, and NCT01653717). CAR+T cells were subsequently electroporated with in vitro–transcribed mRNA encoding the obligate heterodimeric variants of the HLA-A ZFNs. ZFN treatment successfully disrupted HLA-A2 expression in CAR+ T cells without selection, and this population was readily enriched to ∼99% HLA-A2neg cells by negative selection for HLA-positive cells (Figure 5A). These cells were shown to maintain this new phenotype, as after 50 days of continuous coculture on CD19+ aAPC, ∼94% of the CAR+T cells remained HLA-A2neg (not shown). Importantly, these HLA-A2neg T cells evaded attack by HLA-A2-restricted CTL (Figure 5B) and maintained their antitumor activity, as evidenced by CAR-dependent lysis of CD19+ tumor targets (Figure 5C-D).
Loss of HLA-A expression on primary CD19-specific CAR+T cells genetically edited with ZFNs. (A) Disruption of HLA-A2 in CAR+T cells by electro-transfer of mRNA encoding ZFNs. T cells from a HLA-A2+ donor were electroporated and propagated to express CD19-specific CAR (CD19RCD28). These T cells were re-electroporated with 2.5 μg of each mRNA encoding the heterodimeric FokI domain variants of the HLA-A-specific ZFNs (ZFN-L-EL and ZFN-R-KK). HLA-A2 expression was analyzed after culturing at 30°C for 3 days, followed by 37°C for 1 day. Enrichment of the HLA-A2neg population was performed by paramagnetic selection. (B) HLA-Aneg CAR+T cells evade lysis by HLA-A2-restricted CTL. Pools of the indicated CAR+T cells were pulsed with serial dilutions of cognate peptide before being used as targets in a CRA. CTL clone GAS2B3-5, which is specific for C19ORF48/A2, was added at an effector-to-target ratio of 20:1. (C) ZFN-modified HLAneg CAR+ T cells maintain desired antigen-specific cytotoxicity. Redirected specificity for CD19 by HLA-Aneg T cells expressing CD19RCD28CAR was demonstrated using the mouse T-cell line EL4 genetically modified to express a truncated variant of human CD19. Expression of introduced human CD19 on EL4 was 100%. (D) HLAneg CAR+ T cells maintain cytotoxicity against CD19+malignant cells. Cytotoxicity of HLA-Aneg CD19-specificCAR+ T cells was evaluated against CD19+ cell lines (NALM-6 and Daudi) and primary lymphoma cells derived from patients. Data shown are from an effector-to-target ratio of 10:1. Primary cells from DLBCL are diffuse large B-cell lymphoma, and those from MCL are mantle cell lymphoma.
Loss of HLA-A expression on primary CD19-specific CAR+T cells genetically edited with ZFNs. (A) Disruption of HLA-A2 in CAR+T cells by electro-transfer of mRNA encoding ZFNs. T cells from a HLA-A2+ donor were electroporated and propagated to express CD19-specific CAR (CD19RCD28). These T cells were re-electroporated with 2.5 μg of each mRNA encoding the heterodimeric FokI domain variants of the HLA-A-specific ZFNs (ZFN-L-EL and ZFN-R-KK). HLA-A2 expression was analyzed after culturing at 30°C for 3 days, followed by 37°C for 1 day. Enrichment of the HLA-A2neg population was performed by paramagnetic selection. (B) HLA-Aneg CAR+T cells evade lysis by HLA-A2-restricted CTL. Pools of the indicated CAR+T cells were pulsed with serial dilutions of cognate peptide before being used as targets in a CRA. CTL clone GAS2B3-5, which is specific for C19ORF48/A2, was added at an effector-to-target ratio of 20:1. (C) ZFN-modified HLAneg CAR+ T cells maintain desired antigen-specific cytotoxicity. Redirected specificity for CD19 by HLA-Aneg T cells expressing CD19RCD28CAR was demonstrated using the mouse T-cell line EL4 genetically modified to express a truncated variant of human CD19. Expression of introduced human CD19 on EL4 was 100%. (D) HLAneg CAR+ T cells maintain cytotoxicity against CD19+malignant cells. Cytotoxicity of HLA-Aneg CD19-specificCAR+ T cells was evaluated against CD19+ cell lines (NALM-6 and Daudi) and primary lymphoma cells derived from patients. Data shown are from an effector-to-target ratio of 10:1. Primary cells from DLBCL are diffuse large B-cell lymphoma, and those from MCL are mantle cell lymphoma.
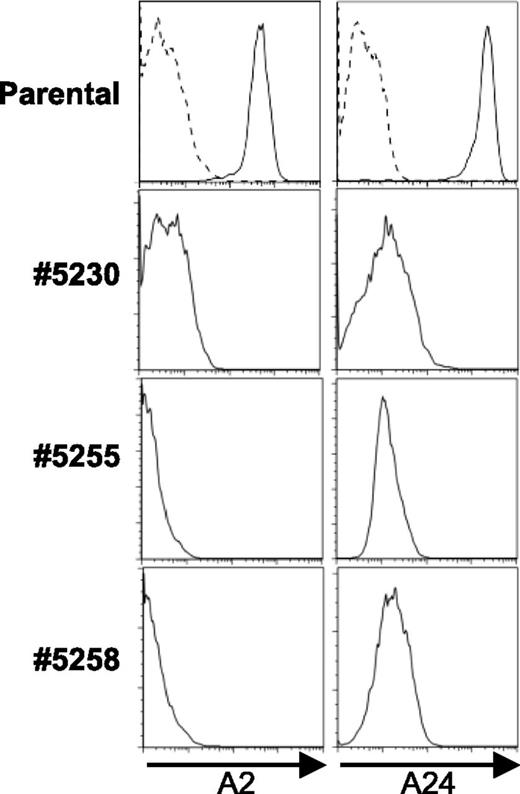
Disruption of the HLA-A in hESCs
To broaden the application of allogeneic cells for therapeutic applications, including tissue regeneration, we sought to generate hESCs capable of evading T-cell recognition. By definition, all hESCs are allogeneic with respect to potential recipients and, on differentiation, will upregulate expression of HLA.38 We genetically modified the HLA-A2+/A24+ hESC line WIBR3 with either mRNAs or DNA plasmids encoding ZFNs targeting HLA-A to evaluate the use of ZFNs for the generation of HLA-AneghESC. To facilitate generation of HLA-AneghESC, we codelivered a donor DNA plasmid encoding the puromycin resistance gene flanked by regions of homology surrounding the ZFN target site to mediate targeted integration by homology-directed repair (supplemental Figure 4). Puromycin-resistant clones were screened for modification of the HLA-A alleles by PCR sequencing of the ZFN target region and by Southern blot analysis of the targeted region, using probes located outside the donor homology groups. These clones, containing mutations in the ZFN target region in both HLA-A alleles, were differentiated into fibroblast-like cells and compared with a similarly differentiated unmodified parental hESC line. HLA expression was induced by treatment with IFN-γ and TNF-α and analyzed by flow cytometry. Although the parental cell line exhibited strong expression of both HLA-A alleles, all 3 knockout lines lacked cell surface expression of both HLA-A alleles (Figure 6). These data demonstrate the portability of the HLA-A knockout approach to hESCs, which may be a necessary step for persistence of these cells and their progeny posttransplantation.
ZFN-mediated elimination of HLA-A expression on human ESC. The HLA-A2+HLA-24+hES parental cell line WIBR3 was modified by ZFN and donor plasmid coding for antibiotic resistance. Clones (5230, 5255, 5258) were chosen with loss of HLA-A expression and differentiated into fibroblasts. Expression of HLA-A2 and HLA-A24 on derived fibroblasts was assessed by flow cytometry after culturing with 600 IU/mL IFN-γ and 10 ng/mL TNF-α for 48 hours. Dashed line in parental panel represents isotype control.
ZFN-mediated elimination of HLA-A expression on human ESC. The HLA-A2+HLA-24+hES parental cell line WIBR3 was modified by ZFN and donor plasmid coding for antibiotic resistance. Clones (5230, 5255, 5258) were chosen with loss of HLA-A expression and differentiated into fibroblasts. Expression of HLA-A2 and HLA-A24 on derived fibroblasts was assessed by flow cytometry after culturing with 600 IU/mL IFN-γ and 10 ng/mL TNF-α for 48 hours. Dashed line in parental panel represents isotype control.
Discussion
A strategy to prevent rejection by the recipient of an allograft without the need to suppress host immunity or confine transplanted cells to privileged sites avoiding immune surveillance would significantly broaden the transplantation of clinical-grade allogeneic cells. However, to prevent donor-derived cells from being recognized by resident T cells, a graft would need to be devoid of expression of mismatched HLA, as antigen-specific TCRαβ can be activated by as few as 3 to 5 peptide/HLA complexes on the target cell.39 Indeed, the potential for immune-mediated rejection is further compounded by the high precursor frequency of allo-reactive T cells (1 in 103-104).40 We provide the proof of principle that ZFNs can target multiple HLA-A alleles for the complete and permanent elimination of HLA-A expression, resulting in cells that can evade T-cell recognition. We observed no apparent detrimental effects on cell growth or function of genome-edited T cells or hESCs as a result of ZFN treatment per se or because of the elimination of HLA-A expression itself. Indeed, T cells expressing a CAR that recognizes CD19, independent of HLA, have shown antitumor effects2,3,33,34,41 and retained their antitumor activity when edited to be HLA-A-negative, suggesting that the ZFN and CAR technologies could be combined to generate off-the-shelf cellular immunotherapy options for patients with cancer.
While increasing the complexity associated with genetically editing multiple loci, the therapeutic strategy to generating off-the-shelf or universal T cells may be further enhanced if coupled with the elimination of other HLA class I as well as HLA class II molecules. This may be accomplished by simultaneous transfection of several pairs of ZFNs targeting a variety of genes.42 Indeed, we validated this strategy by simultaneous modification of T cells with ZFNs to prevent expression of both HLA-A and TCR (supplemental Figure 5). This observation supports our future work to eliminate multiple target genes (including classical HLA molecules other than HLA-A) that may be achieved by a single electro-transfer event of mRNA species encoding multiple ZFNs.
The clinical application of infusing HLAneg cells is appealing, as a single-donor–derived allograft can be preprepared for transfer across transplantation barriers into multiple recipients. This may be achieved by enriching for HLAneg cells or taking advantage of in vivo selection after administration because of immune-mediated recognition and elimination of remaining disparate HLA+ unmodified cells. An additional potential clinical application of allogeneic cell transplantation is engraftment of cells derived from hESCs. These pluripotent stem cells are self-renewing, and yet can be differentiated in vitro into a range of cell and tissue types with the potential to support for cell replacement therapies. However, transplantation of hESCs, which by their definition are allogeneic with respect to the recipient, is complicated by the expression of disparate HLA on derived cells and tissues. We demonstrated a potential solution to this problem; namely, the use of ZFNs to permanently eliminate the expression of specific HLA molecules from the cell surface and thus prevent immune recognition of these epitopes. Even autologous induced pluripotent cells (iPSCs) may benefit from this approach, as T-cell mediated rejection of iPSC derivatives can result from the presentation of immunogenic antigens in the context of HLA.43
Immune-mediated pressure on selecting for HLA expression is noted in some patients with idiopathic aplastic anemia who exhibit loss of heterozygosity of chromosome 6p, resulting in the loss of 1 HLA haplotype.44 In these patients, HLA loss among populations of hematopoietic stem cells apparently leads to immune escape from pathogenic T cells recognizing auto-antigens and results in sustained and functional hematopoiesis. In addition, this loss of HLA did not appear to trigger recognition of hematopoietic stem cells exhibiting loss of heterozygosity by endogenous NK cells. Thus, absence of HLA expression does not necessarily result in NK-cell–mediated lysis.
A concern for loss of classical HLA class I expression is that this may render some allogeneic cells as targets for NK-cell–mediated cytotoxicity based on absence of ligands for KIR.45 A potential solution to this issue may be expression of nonclassical HLA class I molecules such as HLA-E or HLA-G, which have been shown to protect cells from NK-cell–mediated lysis46-49 and are much less polymorphic than classical HLA. Indeed, we have validated the approach of preventing NK-cell lysis by enforced expression of HLA-E and/or HLA-G on the HLA class Inull721.221 cell (supplemental Figure 6). This provides a solution to forestall elimination of administered HLAneg allogeneic cells by recipient NK cells.
In summary, we demonstrate that transformed, primary, and pluripotent stem cells can be permanently modified by ZFNs to eliminate HLA-A expression. Our approach has the potential for rapid application in humans, as we employ mRNA electroporation (a process with growing use in GMP manufacturing of cellular products), resulting in the transient expression of ZFNs (which as a class have already been taken to the clinic). The ability to generate a priori cells from a single allogeneic donor to be infused across transplantation barriers into multiple recipients represents a significant step toward our goal of on-demand therapy with universal cells that can be predeployed at multiple sites and infused when needed, rather than when the cells are available.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank C. June (University of Pennsylvania) for help generating and providing aAPC clone 4; M. Fernández-Viña (Stanford University) for his assistance with HLA-typing and providing antibody; A. Multani (MD Anderson Cancer Center) for her assistance with karyotyping; L. Zhang, S. Hinkley, and A. Vincent (Sangamo Biosciences) for generation of the ZFN reagents; S. Abrahamson (Sangamo Biosciences) for editing the manuscript; and E. Lanphier (Sangamo Bioscience) for encouragement and support. The Cancer Center Support Grant core-supported facilities “Characterized Cell Line Core” undertook fingerprinting of cell lines.
This work was supported by grants from the Cancer Center (CA16672); R01 (CA124782, CA120956, CA141303; CA141303); R33 (CA116127); P01 (CA148600); Burroughs Wellcome Fund; Cancer Prevention and Research Institute of Texas; Caryn Papantonakis; CLL Global Research Foundation; DARPA (Defense Sciences Office); Department of Defense; Estate of Noelan L. Bibler; Gillson Longenbaugh Foundation; Harry T. Mangurian, Jr, Fund for Leukemia Immunotherapy; Institute of Personalized Cancer Therapy; Leukemia and Lymphoma Society; Lymphoma Research Foundation; The MD Anderson Cancer Center’s Sister Institution Network Fund; Miller Foundation; Mr Herb Simons; Mr and Mrs Joe H. Scales; Mr and Mrs Rick Calhoon; Mr Thomas Scott; National Foundation for Cancer Research; Paula Gavrel Asher Foundation; Pediatric Cancer Research Foundation; Robert J. Kleberg, Jr and Helen C. Kleberg Foundation; Uehara Memorial Foundation; and William Lawrence and Blanche Hughes Children's Foundation. This work was also supported by grants from the National Institutes of Health (R37, CA084198; and R01, CA087869 and HD045022 to R.J.).
Authorship
Contribution: H.T., A.R., and F.S. designed, performed experiments, analyzed the data, and wrote the paper; C.Y., Y.Z., D.L.C., J.C.M., N.L., and Z.Z. performed experiments; E.H.W. and S.S.T. provided CTL clones; H.H. coordinated experiments; E.J.R., P.D.G., and M.C.H. designed experiments and wrote the paper; P.K., D.A.L., and R.E.C. analyzed the data; R.J. designed experiments and analyzed the data; and L.J.N.C. conceived the idea, coordinated the project, designed experiments, and wrote the paper.
Conflict-of-interest disclosure: A.R., Z.Y., N.L., Z.Z., J.C.M., M.C.H., E.J.R., P.D.G. are current (or former) employees of Sangamo BioSciences Inc. The remaining authors declare no competing financial interests.
Correspondence: Laurence J. N. Cooper, The University of Texas MD Anderson Cancer Center, Pediatrics, Unit 907, 1515 Holcombe Blvd, Houston, TX 77030; e-mail: ljncooper@mdanderson.org.