In this issue of Blood, Shi and coworkers show that TNT003, a mouse monoclonal antibody targeting complement protein C1s, prevents induction of in vitro hemolysis by cold agglutinins (CA).1 If successfully transferred into the clinical setting by further studies, these findings may result in a novel therapeutic principle for a frequently difficult problem.
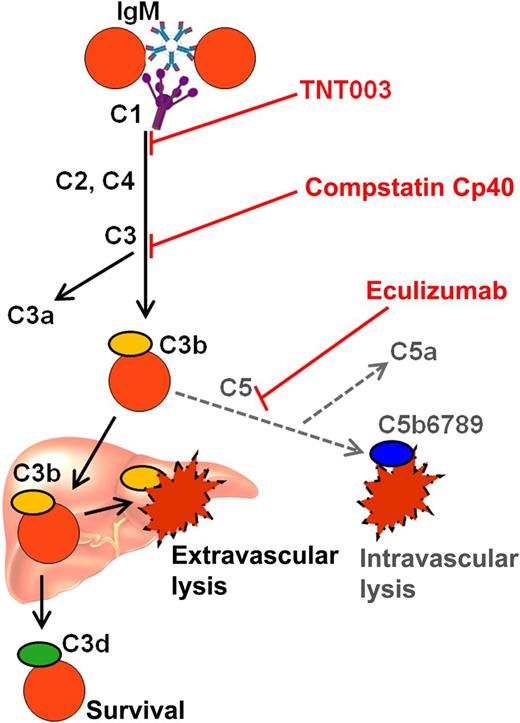
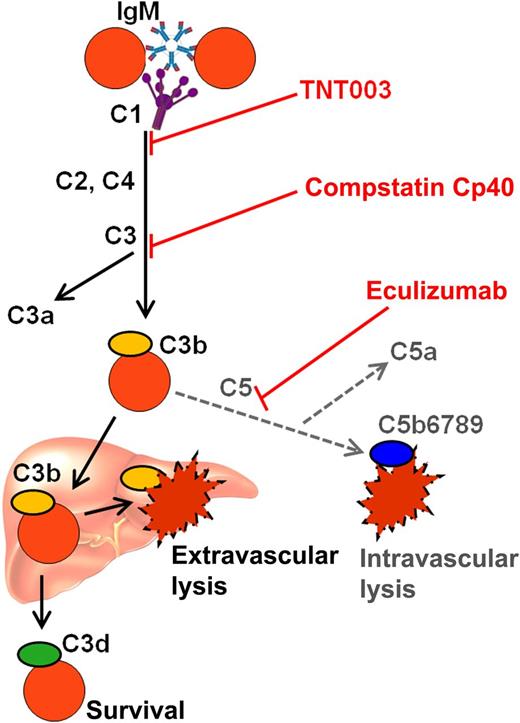
Complement-mediated destruction of erythrocytes in CAD and possible targets for complement-directed therapy. C, complement protein; IgM, immunoglobulin M.
Complement-mediated destruction of erythrocytes in CAD and possible targets for complement-directed therapy. C, complement protein; IgM, immunoglobulin M.
Primary chronic CA disease (CAD) is the “least uncommon” type of cold-antibody autoimmune hemolytic anemia (AIHA), accounting for about 15% of AIHA. Recent studies have shown that CAD is a well-defined clinicopathologic entity, characterized by a probably distinct clonal lymphoproliferative B-cell disorder of the bone marrow.2 The autoimmune hemolysis in CAD is entirely dependent on complement activation by the classical pathway (see figure). C3b opsonized erythrocytes are phagocytosed by reticuloendothelial cells, predominantly in the liver, resulting in extravascular hemolysis.3 According to the prevailing view, activation of the terminal complement pathway with intravascular hemolysis is usually not important but does occur in some patients and situations, as evidenced, for example, by the finding of hemoglobinuria in 15% of the patients.4,5 Secondary CA syndrome (CAS) associated with specific infections or aggressive lymphoma is a heterogeneous condition, different from CAD in terms of etiology and B-cell clonality but characterized by the same complement-dependent mechanism of hemolysis.
The anemia in CAD is not always mild, as shown by the lower tertile hemoglobin level of 8.0 g/dL.4 Furthermore, acute-phase reaction in febrile diseases or following major surgery or trauma may result in complement-mediated, sometimes severe exacerbations.6 In a cool climate, approximately 90% of the patients experience cold-induced circulatory symptoms that are caused by red cell agglutination and are, therefore, complement independent.4 In descriptive studies from Norway as well as the United States, pharmacologic therapy had been attempted in 70% to 80% of the patients.4,5
The relative success in treatment of CAD during the last decade has been achieved through targeting the pathogenic B-cell clone. Rituximab monotherapy has produced approximately 50% response rates, whereas the combination of rituximab and fludarabine has resulted in a 75% response rate, 20% complete responses, and median response duration of more than 66 months.7,8
Shi and coworkers tested the in vitro effects of TNT003 on CA-induced complement activity against human erythrocytes.1 This monoclonal antibody has specificity for the complement serine protease C1s. Using CA samples from 40 patients with CAD, they found that TNT003 prevented CA-induced deposition of C3 fragments on the erythrocytes at the same concentration of antibody that stopped hemolysis. The inhibition of C1s also resulted in prevention of in vitro erythrophagocytosis by a phagocytic cell line. Furthermore, TNT003 inhibited the CA-induced, classical–pathway-driven generation of anaphylatoxins C4a, C3a, and C5a. Interestingly, CA from only 1 patient sample out of 40 was able to directly induce membrane attack complex (MAC)-mediated hemolysis. The findings support the existing view that complement activity in CAD terminates prior to activation of the terminal pathway in most patients.
TNT003 is not the only complement-inhibiting substance that may be considered for future treatment of CAD. The monoclonal anti-C5 antibody eculizumab is a powerful therapeutic agent in paroxysmal nocturnal hemoglobinuria (PNH). In PNH, however, the predominant route of complement-mediated hemolysis is the intravascular cell destruction caused by activation of the terminal complement pathway, starting with C5 cleavage and resulting in the formation of MAC. It may seem surprising, therefore, that eculizumab therapy did produce major improvement of CAD according to a single case report.9 Further studies can be expected to elucidate this observation. A low-molecular-peptide complement inhibitor that prevents cleavage of C3, compstatin Cp40, has shown promising effects on complement-mediated lysis of erythrocytes from PNH patients.10 Because of the essential role of C3 in CAD as well, further experiments might be expected to show a favorable effect of C3-blocking agents on CA-induced hemolysis.
Given that targeting the pathogenic B-cell clone is an effective and more causal therapeutic approach and immunochemotherapy is administered only for a limited period of time, do we actually need complement-directed therapies for CAD? First, after all, immunochemotherapy is unsuccessful in at least 25% of the patients because of treatment failure or toxicity.8 The pathogenic B-cell clone can be small with low proliferation activity and, therefore, difficult to target efficiently.2,4 Second, rapidly acting therapy seems required in some specific clinical settings. Examples of such situations are acute severe exacerbation induced by febrile infections, major surgery, or trauma and, possibly, before cardiac surgery in selected patients. Anticomplement therapy might also prove useful in severe cases of secondary CAS. Because complement is not involved in the agglutination of erythrocytes, complement inhibition cannot be expected to improve the cold-induced circulatory symptoms, which are of major clinical importance in some patients with CAD.
The further road toward clinical application is probably not straightforward. Starting with TNT003, a corresponding humanized monoclonal antibody will have to be developed. Perhaps more difficult, inhibition of the complement system will carry a risk of infection. Based on comprehensive clinical data on eculizumab, the risk of infection resulting from C5 inhibition is known to be negligible provided the patients can be efficiently protected against meningococci. Blocking the complement system at a more proximal level may pose a much higher risk. Efficient inhibition of C3 by compstatin Cp40 will completely block complement activation beyond this level, whether initiated by the classical, alternative, or lectin pathway.10 Interestingly, however, the still more proximal blockade achieved by TNT001 will only block the classical pathway as required for the treatment of CAD.1 Thus, the alternative and lectin pathways will remain intact and will be able to activate the terminal pathway as well as the production of anaphylotoxin C3a in response to microbial stimuli. Although this selectivity may reduce the risk of infection, careful investigations will be required to address this issue.
New complement-modifying agents that prove useful in CAD are of potential interest in other complement-mediated diseases, too, depending on the details of complement involvement. Clinical studies of such drugs are probably not far ahead.
Conflict-of-interest disclosure: The author declares no competing financial interests.