In this issue of Blood, Sorror and coworkers report that pretransplant comorbidities predict the severity of acute graft-versus-host disease (aGVHD) and associated treatment-related mortality following hematopoietic stem cell transplantation (HSCT).1
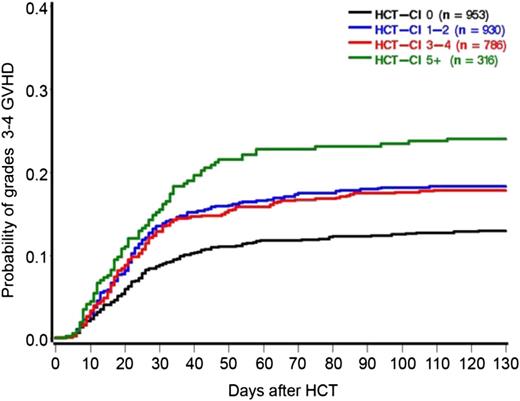
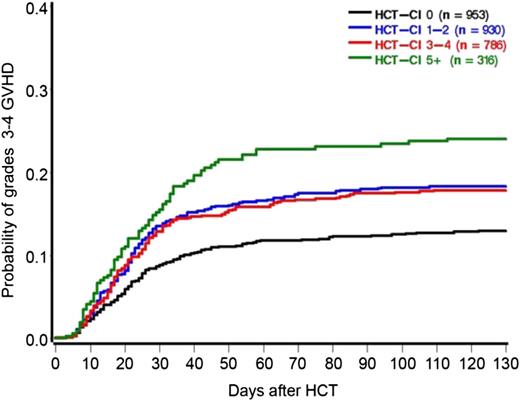
Cumulative incidence of grade 2 to 4 aGVHD depending on pretransplant HCT-CI. See Figure 1 in the article by Sorror et al that begins on page 287.
Cumulative incidence of grade 2 to 4 aGVHD depending on pretransplant HCT-CI. See Figure 1 in the article by Sorror et al that begins on page 287.
aGVHD is induced by alloreactivity of donor T-cells against recipient (host) tissues. It requires genetic disparity between donor and recipient. Tissue injury occurs both from direct T-cell cytotoxicity and production of inflammatory cytokines.2 Risk factors for development of aGVHD include HLA disparity, use of unrelated donors, and donor alloimmunization.3-5 Viral infections such as cytomegalovirus may produce immune activation leading to development of GVHD.6
The severity of the clinical syndrome of aGVHD is scored by the extent of target organ injury, assessed by the extent of skin rash, diarrhea, and hyperbilirubinemia.7 The ultimate aGVHD score reflects damage due to alloreactivity superimposed on any coexisting organ injury due to comorbid diseases, infections, and the toxicity of the preparative regimen.8
Sorror et al9 have previously demonstrated that the pretransplant hematopoietic cell transplantation-comorbidity index (HCT-CI) is a predictor of nonrelapse mortality after allogeneic HSCT. In this study, they examine the associations between the pretransplant HCT-CI and development of aGVHD and associated nonrelapse mortality. They examined the outcomes of 2985 patients with myeloid and lymphoid malignancies who received both myeloablative and reduced intensity conditioning for HSCT. Increasing HCT-CI score was significantly associated with an increased risk for grades 2 to 4 and grades 3 to 4 aGVHD in multivariable analysis. This effect was seen for myeloablative and nonmyeloablative conditioning, related and unrelated donor transplants, and peripheral blood and bone marrow grafts.
HCT-CI scores could be collapsed into 3 risk groups for prediction of grades 3 to 4 aGVHD; 0 vs 1 to 4 vs ≥5 (see figure).1 The time to development of aGVHD was also shorter in patients with a higher HCT-CI. Patients with the highest comorbidity scores were predominantly older. However, age was not statistically significantly associated with increased risks for grades 3 to 4 aGVHD in the regression model.
The specific types of comorbidity may be important. The low sample sizes for individual comorbidities limited the power to detect significant relationships, but the greatest relative risk for GVHD was in patients with preexisting liver disease, rheumatologic conditions, inflammatory bowel disease, and infections, disorders that could increase inflammation and damage to the target organs.
It stands to reason that patients with greater preexisting morbidity would have a higher rate of mortality if they develop major complications of hematopoietic transplantation. Indeed, patients in this study with a greater HCT-CI had a higher mortality if they developed grade 2 to 4 aGVHD. Higher mortality has also been reported to be related to the HCT-CI in transplant recipients requiring intensive care after HSCT.10
How should we use this information? Selection of patients for HSCT requires understanding both the risks and potential benefits of this treatment modality. This study demonstrates that patients with high comorbidity scores have higher rates of the major morbidity, aGVHD, and nonrelapse mortality, as well as the magnitude of these risks.
Conflict-of-interest disclosure: The author declares no competing financial interests.