Abstract
The safety and efficacy of graft-versus-host disease (GVHD) prophylaxis with high-dose cyclophosphamide (pCY) given after allogeneic bone marrow transplantation from HLA-haploidentical and HLA-matched related and unrelated donors has been reported in several studies. We hypothesized that pCY would reduce the incidence of severe acute and chronic GVHD with low toxicity and effective disease control after transplantation of G-CSF-mobilized blood cells from HLA-matched related and unrelated donors. The study was designed to provide at least 90% power to observe a reduction in the incidence of chronic GVHD requiring systemic treatment from 35% to ≤ 15% with a one-side type-1 error of ≤ 5%.
Forty-three patients (median age 38, range 3-66) with high-risk hematologic malignancies (acute myeloid leukemia, n=18; myelodysplastic syndrome, n=9; acute lymphoblastic leukemia, n=12; chronic myeloid leukemia, n=3, and lymphoma, n=1) were enrolled at a single center between December 2011 and September 2013. Thirty-one (72%) patients had disease in remission, and 12 (28%) had residual or progressive disease at the time of transplant. Twelve (28%) patients received grafts from related donors, and 31 (72%) received grafts from unrelated donors. Pretransplant conditioning consisted of high-dose busulfan in combination with fludarabine (n=25) or high-dose total body irradiation (12-13.2 Gy; n=18). pCY at 50 mg/kg/day was given on days 3 and 4 after transplantation, followed by cyclosporine starting on day 5 (target level, 120-360 ng/mL). In the absence of GVHD, cyclosporine doses were tapered from day 56 through day 126.
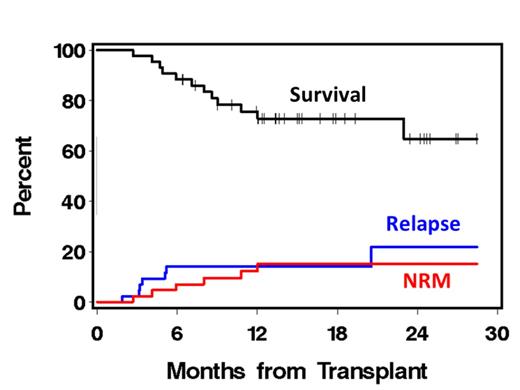
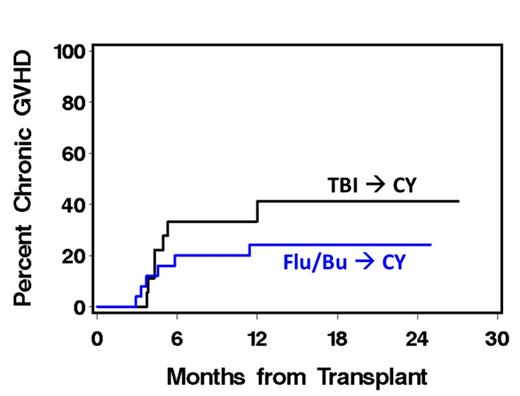
The cumulative incidences of grade II-IV acute, grade III-IV acute, and chronic GVHD were 77%, 0%, and 31%, respectively. Non-relapse mortality (NRM) at 100 days and 1 year was 2% and 15%, respectively. The incidence of recurrent malignancy at 1 year was 14%. With a median follow-up of 15 months, the two-year overall survival rate was 65%. Patients prepared with busulfan and fludarabine had a lower incidence of chronic GVHD compared to those prepared with total body irradiation (24% vs 41%; p=0.37) even though the median age of patients in the former group was substantially higher than in the latter group (52 vs 23.5 years).
This study demonstrates that although myeloablative pretransplant conditioning with busulfan/fludarabine or total body irradiation can be safely combined with pCY and cyclosporine, the risk of chronic GVHD with mobilized blood cell grafts is higher than previously reported with marrow grafts. This finding suggests that with HLA-matched related or unrelated donors, depletion of alloreactive T cells by pCY is insufficient to prevent chronic GVHD, possibly reflecting the larger number of T cells in mobilized blood cell grafts as compared to marrow grafts, or lower sensitivity of T cells exposed to G-CSF in vivo as compared to resting T cells.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.