Abstract
Some studies that evaluated the predictive value of lung function prior to allogeneic hematopoietic stem cell transplant (allo-SCT) showed a statistically significant relationship between pulmonary function test (PFT) parameters and outcome. However, patients infrequently display significant abnormalities in lung function before allo-SCT, specifically forced expiratory volume in one second (%FEV1.0) and vital capacity (%VC). In addition, the underlying mechanism for the abnormalities in PFT parameters present before allo-SCT remains elusive.
V50/V25 ratio is known to be a sensitive marker of small airway obstruction and an abnormal V50/V25 ratio often becomes detectable even in patients in whom %FEV 1.0 and/or %VC are normal. To our knowledge, nobody has reported the effect of the V50/V25 ratio on outcome in patients undergoing allo-SCT.
We here comprehensively evaluate the effect of PFT parameters determined before allo-SCT on survival and outcomes. We also address the causes of deterioration in PFT indicators. We retrospectively studied 159 evaluable patients who received allo-SCT at our institute between June in 2004 and December in 2012, and who had available PFT data acquired before allo-SCT (median age 46). The median follow-up duration for survivors was 875 days. We evaluated PFT indicators including %VC, %FEV1.0, MMF, %RV, RV/TLC, FVC, FEV1.0/FVC, DLco/VA, V25 and V50/V25 ratio. Analysis using a univariate Cox proportional hazard model showed that %VC, %FEV1.0, DLco/VA, RV/TLC, and V50/V25 ratio (all P< 0.05) were significantly compromised in patients who died. On multivariate analysis, %VC, DLco/VA and V50/V25 retained statistical significance (all P-<0.01). Notably, among these significant parameters, V50/V25 was found to be the most sensitive and powerful indicator of survival after allo-SCT (HR: 2.15 per 1-SD-magnitude, 95% CI: 1.53-3.03, P<0.0001). In addition, 56% of all patients had an abnormal V50/V25 (>3.0) pre allo-SCT, whereas in just 12% and 11% respectively were the %FEV1.0 (< 80%) and %VC (< 80%) abnormal. Moreover, the V50/V25 determined before allo-SCT was significantly correlated with age (P <.001) and smoking history (P <.05) but not type of disease, disease status, performance status, intervals between diagnosis and transplantation.
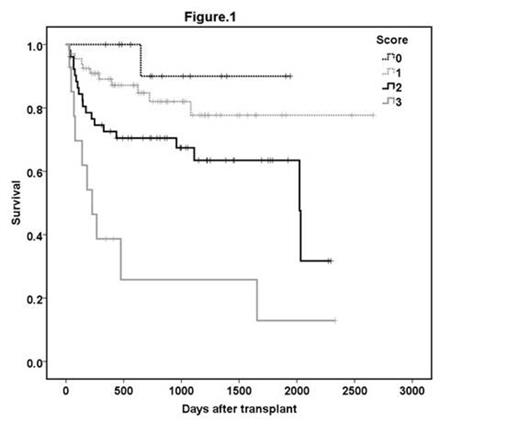
Next, we established a scoring system for lung function by applying three independently significant parameters. Importantly, the three indicators for which statistical significance was detected have distinct physiological implications. V50/V25 is a marker of obstruction, %VC, a measure of lung capacity, and diffusing capacity for carbon monoxide/alveolar volume (DLco/VA), a measure of diffusing capacity. We assigned a separate score (%VC; < 80% = 1 and > 80% = 0, DLco/VA; < 80% = 1 and > 80% = 0, V50/V25; >3.25=1 and < 3.25 = 0) and stratified all patients into the four group by total score. The scoring system consisting of %VC, DLco/VA and V50/V25 represented a significant discriminating variable for prediction of survival after allo-SCT (Figure 1).
In the current study, our data demonstrate the predictive value of a sensitive small-airway disease indicator, V50/V25, for survival. Although we cannot exclude the presence of other potential factors affecting V50/V25 in hematological patients, our results demonstrate that V50/V25 might be significantly compromised by age, and/or smoking before allo-SCT. In addition a scoring system that incorporates V50/V25 instead of %FEV1.0 may be a potentially useful clinical tool for prediction of survival after allo-SCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.