Abstract
Introduction: Follicular lymphoma (FL) is the most common indolent non-Hodgkin lymphoma. Though no agreed upon standard of care has been established, the incorporation of immunotherapy has been widely adopted given a number of studies demonstrating improvement in response rates, progression-free survival (PFS), and overall survival (OS) with the addition of rituximab. The most common frontline management strategy in the United States (US) for FL is chemoimmunotherapy. However, there is significant heterogeneity in practice patterns, and the relationships between insurance status, chemoimmunotherapy use, and survival in patients (pts) with FL across the US remain unclear. We utilized a national cohort of adult pts with long-term follow-up of FL to test the hypotheses that uninsured patients are less likely to receive chemoimmunotherapy and more likely to experience poorer OS even after controlling for socieodemographic factors, clinical factors, and treatment.
Methods: We used data from the National Cancer Data Base (NCDB), a nationwide oncology outcomes database jointly sponsored by the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. Begun in 1989, NCDB currently contains approximately 29 million records from hospital cancer registries covered by more than 1,500 CoC-accredited cancer programs in US and Puerto Rico. Approximately 75% of all newly diagnosed cancer cases in the US are captured. Data collection by CoC-accredited cancer program uses national standardization, and vital status and date of death are reported to the NCDB on a yearly basis.
Pts with FL were identified using the International Classification Oncology (ICD-O) histology codes 9690, 9691, 9695, 9698. The population was restricted to pts diagnosed in 2004, adults age 18-101, and those who received all/part of their first course of treatment at the reporting facility. Cases with missing data (age, gender, race, region, insurance data, treatment) and those with non-Medicare/Medicaid government insurance (VA, Indian Health Services) were removed. Pts with HIV, ≥65 years of age, or aged <65 years whose primary insurance was Medicare were also removed. All information was captured using standardized codes defined by the Facility Oncology Registry Data Standards (FORDS). Chi-square tests were used to compare clinical characteristics by insurance status. Log-binomial models were fitted to examine the association of insurance status with clinical factors including advanced stage (III/IV), presence of B-symptoms, comorbidities, and receipt of chemoimmunotherapy. Kaplan-Meier survival curves and log-rank tests were performed. Multiple variable Cox proportional hazards models examined the contribution of prognostic factors to survival disparity by insurance status.
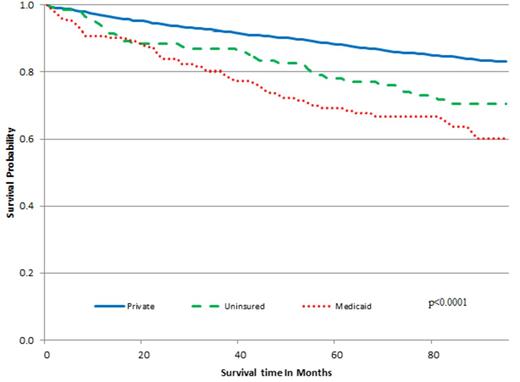
Results: 2,703 pts diagnosed in 2004 in the NCDB met inclusion criteria. Compared with privately insured pts, uninsured or Medicaid insured pts were more likely to have advanced stage disease and B symptoms, but no significant difference in the presence of comorbidities. Compared with privately insured pts, there were no differences in chemoimmunotherapy use for uninsured patients, but Medicaid insured pts were more likely to receive chemoimmunotherapy (Medicaid risk ratio [RR] 1.41; 95% confidence interval [CI] 1.09-1.82). Medicaid and uninsured pts had a significantly higher risk of death compared with privately insured pts even after controlling for socieodemographic, prognostic, and treatment factors (uninsured hazard ratio [HR] 1.78; 95% CI 1.24-2.54; Medicaid HR 2.50; 95% CI 1.84-3.39). Disease stage, age, sex, residing in an area with > 20% of residents not graduating from high school, the presence of B symptoms, and comorbidities, but not treatment were significant, independent predictors of survival in pts with FL and contributed to the disparities in survival by insurance status.
Conclusions: Although uninsured and Medicaid insured pts with FL in the US did not have lower use of chemoimmunotherapy, both groups had inferior survival compared to privately insured pts. Despite heterogeneity in management strategies for FL, access to adequate health care has the potential to improve survival for pts with FL.
Overall survival of FL patients by insurance status, NCDB 2004
Overall survival of FL patients by insurance status, NCDB 2004
Nastoupil:Genentech: Honoraria; Celgene: Honoraria; TG Therapeutics: Research Funding; Janssen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.