Abstract
Purpose:
The purpose of this study was to examine whether quality of life (QOL) scores at diagnosis predict survival among patients with aggressive lymphoma, controlling for clinical variables and histological subtype.
Patients and Methods:
Newly diagnosed lymphoma patients were prospectively enrolled within 9 months of diagnosis in the University of Iowa/Mayo Clinic SPORE Molecular Epidemiology Resource. Eligibility criteria included age ≥18 years; exclusion criteria included HIV-positive, non-US residency, and inability to participate in an interview conducted in the English language. All pathology was reviewed by a lymphoma hematopathologist. For purposes of this analysis, we considered aggressive lymphoma to include the histological subtypes diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL) grade III, mantle cell lymphoma, T-cell lymphoma excluding mycosis fungoides and cutaneous types, and other (Burkitt lymphoma, high grade B-cell lymphoma NOS, grey zone, etc). Baseline QOL was measured at time of registry enrollment with the Functional Assessment of Cancer Treatment-General scale (FACT-G), which measures 4 QOL domains: physical, social/family, emotional, and functional well-being (WB); a single item Linear Analogue Self Assessment (LASA) for measuring overall QOL; and a LASA measuring spiritual WB. Patients who did not complete ≥80% of FACT-G QOL questions were excluded. Clinical data were abstracted and patients were systematically followed for event-free and overall survival (EFS, OS). QOL scores were transformed to a 0-100 scale for modeling. Generalized additive models were used to account for timing of QOL assessment in relation to treatment and diagnosis; residuals from these models were then used to assess association between QOL measures and outcome via univariate and multivariable (adjusted for IPI and subtype) Cox proportional hazards models.
Results:
From September 2002 to December 2009, 701 patients with aggressive lymphoma who completed baseline QOL questionnaires were enrolled and eligible for this analysis. ; Subtype was 60% DLBCL, 14% mantle cell, 11% FL grade III, 13% T-cell, and 1% other subtypes. The median age was 62 years (range 18-92), and 58% were male. At a median follow-up of 71 months (range 6-128), 316 patients (45%) had an event and 228 patients (33%) died. Patient-reported QOL was prior to therapy in 330 patients (47%) and after initiation of therapy in 371 (53%). The median overall FACT-G total score was 83 (IQR 70-93), and the median scores on the functional WB, physical WB, emotional WB, and social/family WB were 18 (13-23), 22 (17-26), 18 (16-21), and 25 (22-27), respectively. 42 patients (6%) reported a clinically deficient QOL score on the FACT-G (score ≤50 on 0-100 scale). When comparing QOL scores between those who were on active therapy versus those who were not yet treated, physical WB (p<0.0001) functional WB (p=0.00014), and total FACT-G (p=0.0013) were lower in those on active treatment.
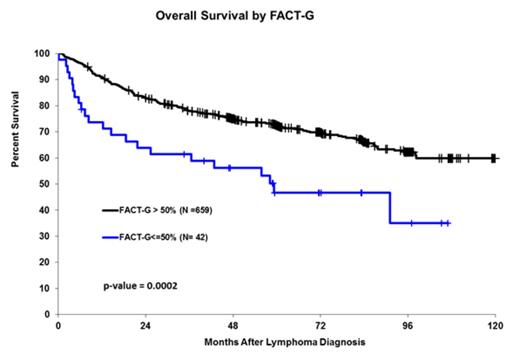
All QOL measures but emotional WB were significantly associated with OS (all p<0.04), and all but LASA spiritual WB remained significant after adjusting for IPI and NHL subtype. Associations were stronger for OS than EFS. For OS, the strongest associations were with total FACT-G (adjusted HR=0.86, 95% CI: 0.79-0.94, p=0.00062) and functional WB (adjusted HR=0.88, 95% CI: 0.83-0.93, p<0.0001). The one-question QOL LASA was also associated with OS (adjusted HR=0.92, 95% CI: 0.87-0.97, p=0.0041). The strongest association with EFS was with functional WB (adjusted HR=0.92, 95% CI: 0.88-0.97, p=0.0015). Patients with a clinically deficient QOL (baseline overall QOL ≤50) had a median OS of 59 months compared to 121 months for patients with baseline QOL >50, p=0.0002, figure 1.
In a sensitivity analysis, raw QOL was modeled for OS and EFS in the subset of patients with QOL assessed prior to treatment; hazard ratios were consistent with the adjusted QOL HR in all patients.
Conclusions:
In this large sample of patients with aggressive lymphoma, baseline QOL is predictive of OS and EFS, even after adjustment for known factors related to survival (IPI and histological subtype). This provides evidence that patient-reported outcomes are as important as other more objective previously confirmed IPI measures. QOL should be assessed at diagnosis as a prognostic factor in patients with aggressive lymphoma.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.