Abstract
Background: Angiogenesis has previously been shown to contribute to acute graft-versus-host disease (aGVHD) post-allogeneic hematopoietic cell transplantation (HCT), but its association with response to therapy is not known. We hypothesized that patients with abundant circulating angiogenic factors (AF) involved in repair/regeneration would have improved outcomes relative those with higher levels of AF involved in damage/inflammation.
Patients and Methods: We measured by MILLIPLEX magnetic bead array circulating levels of AF known predominantly for repair/regeneration (epidermal growth factor [EGF], fibroblast growth factor (FGF)-1, FGF-2, heparin binding-EGF-like growth factor, follistatin [FS], vascular endothelial growth factor [VEGF]-A, VEGF-C, and VEGF-D) and those known predominantly for endothelial dysfunction/inflammation (angiopoietin-2 [Ang2], endothelin-1, endoglin [sEng], leptin, placental growth factor [PlGF]) in HCT recipients with grade III-IV acute GVHD (N=17) compared to recipients who did not experience aGVHD post-HCT (N=17) and healthy stem cell donors (HD, N=16). AF demonstrating <0.5-fold or >1.5-fold difference in median with p‰¤0.1 in the pilot study were validated in a cohort with aGVHD (N=158) enrolled in Blood and Marrow Transplant Clinical Trials Network (BMT CTN) 0802, with samples analyzed at aGVHD onset and day 28 post-GVHD treatment, compared to allogeneic HCT recipients from the University of Minnesota who did not experience aGVHD (N=53).
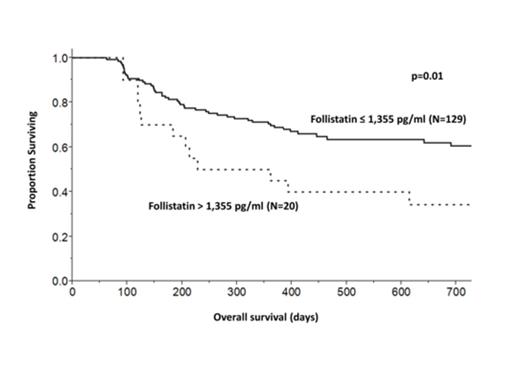
Results: In the pilot study, AF associated with repair/regeneration were altered at aGVHD onset. Specifically, FS was 1.9-fold elevated in patients with aGVHD, while EGF and VEGF-A levels were lower compared to HCT recipients without aGVHD. Three AF that are indicative of damage/inflammation (PlGF, Ang2, and sEng) were elevated in aGVHD patients compared to HD. In the validation cohort (Table), levels of FS were 2-fold higher, and levels of sEng and PlGF were 1.7-fold higher in aGVHD compared to HCT controls. As with the pilot study, levels of EGF and VEGF-A were lower (6-fold and 2.6-fold, respectively) in aGVHD. None of the factors differed by grade or organ stage. Patients who received grafts from matched unrelated donors (URD) had a 50% increase in PlGF levels at aGVHD onset compared to sibling donors HCT with aGVHD (31.3 versus 21.8 pg/mL, p=0.03). Patients with aGVHD who had a complete response (CR) to therapy at day 28 had higher levels of EGF and VEGF-A compared to those who had a partial response or no response (Figure 1). Patients with FS levels >85th percentile (>1,355 pg/mL, Figure 2) had an increased risk of death (RR 2.1, 95% CI 1.1 €“ 3.8, p=0.03).
Conclusions: Three AFs were elevated at aGVHD onset: FS, sEng and PlGF. Elevated FS is associated with shortened survival. Although FS is critical for tissue regeneration after injury, excess FS may reflect more extensive tissue damage or loss and has recently been linked to delayed healing in a rodent model. EGF and VEGF-A levels are low in aGVHD and are higher with CR at day 28, which may reflect improved tissue production or reduced losses. PlGF levels are disproportionately elevated in aGVHD after URD HCT. Further studies are evaluating the impact of these 5 angiogenic factors on healing and the regulation of inflammation post-HCT, with a goal to identify novel, non-immunosuppressive treatments to improve outcomes of aGVHD.
Six angiogenic factors in patients at aGVHD onset compared to those without aGVHD and day 28 post-treatment.
| Factor (median, pg/mL) | Onset (N=158) | No aGVHD (N=53) | Day 28 (N=158) |
| Follistatin | 855 | 445* | 1,022 |
| EGF | 18 | 112* | 15 |
| VEGF-A | 117 | 309* | 137 |
| Endoglin | 1,691 | 1,013* | 1,722** |
| Ang2 | 3,264 | 3,590 | 2,734** |
| PlGF | 26 | 14* | 32 |
| Factor (median, pg/mL) | Onset (N=158) | No aGVHD (N=53) | Day 28 (N=158) |
| Follistatin | 855 | 445* | 1,022 |
| EGF | 18 | 112* | 15 |
| VEGF-A | 117 | 309* | 137 |
| Endoglin | 1,691 | 1,013* | 1,722** |
| Ang2 | 3,264 | 3,590 | 2,734** |
| PlGF | 26 | 14* | 32 |
Compared to onset, *p<0.001 by Mann-Whitney and **p<0.002 by Wilcoxon signed rank.
Levels of circulating EGF and VEGF-A at day 28 by response to aGVHD therapy.
Levels of circulating EGF and VEGF-A at day 28 by response to aGVHD therapy.
Follistatin levels and survival after aGVHD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.