Abstract
Production of abnormal hemoglobin (HbS) in sickle-cell disease (SCD) results in its polymerization in deoxygenated conditions and in sickled-RBC formation. Dense RBCs (DRBCs), defined as density >1.11 and characterized by increased rigidity, viscosity and HbS concentration (main polymerization factor), are absent in normal AA subjects, but present at percentages that vary from 1 SCD patient to another but remain stable throughout adulthood for each patient. Polymerized, but not nonpolymerized, HbS has reduced affinity for oxygen, demonstrated by the rightward shift of the oxygen-dissociation curve, leading to disturbances in oxygen transport. We recently described a correlation between %DRBCs and some clinical SCD manifestations. Notably, some SCD patients have unexplained, very low oxygen saturation (SpO2), without heart or lung dysfunctions. %DRBC variability within SCD patients could be the main pathophysiological explanation of those manifestations. This study was undertaken to determine whether a link exists between the %DRBCs and Hb affinity for oxygen, and to look for a potential clinical implication for SCD patients.
92 patients (44.6 ± 7.7 years; 51 women and 41 men) were included in the study. Blood samples were obtained at steady state to measure hemorheological and hematological parameters. Using a Percoll-gradient fractionation method, total RBCs were separated into non-DRBCs (NDRBC) (d<1.11) and DRBCs (d>1.11) fractions. The %DRBCs was determined using the phthalate-gradient method. P50 in venous blood gases was measured with a radiometry analyzer. Oxygen-affinity curves of Hb dissociation and association in RBC fractions were obtained with dual wavelength spectrophotometry. All patients had a 6-minute walking test (6MWT) and 10 of them (38.1 ± 6.1 years; 6 men and 4 women) had done so before and after >6 months (>6M) on hydroxyurea (HU). Times <90% and <88% transcutaneous SpO2 of Hb and a SpO2 decrease ≥4% during the test (delta SpO2 >4%) were evaluated to investigate the physiological impact on patients during exertion. Patients, divided into quartiles according to their values (Q1: 0–25th centile, Q2–Q3: 25th–75th centiles, and Q4: >75th centile), were analyzed for the times <88% SpO2, <90% SpO2 and with delta SpO2 >4%, for the distance walked.
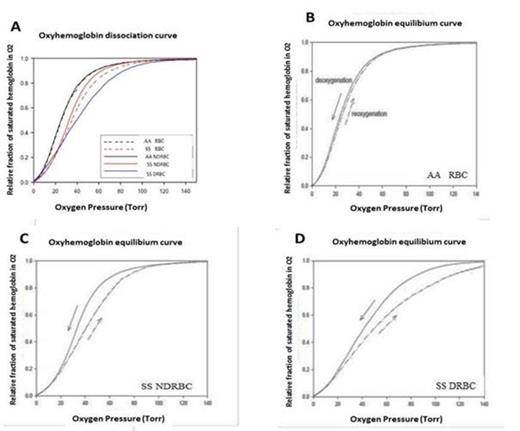
DRBCs had increased MCHC and decreased %HbF and 2,3 DPG, leading to more polymerization and modulation of Hb affinity for oxygen, compared to NDRBCs. Moreover, dissociation and association curves of SS RBC fractions differed (compared to AA RBCs), with rightward shifts of NDRBCs and, more importantly, DRBC-association curves, thereby confirming the role of HbS polymerization in the loss of affinity (Fig 1). Bivariate analysis showed that the P50 was positively correlated with the %DRBCs (P<0.0001, r²=0.34), reflecting a link between the total Hb–oxygen affinity and %DRBCs in SCD patients. Conversely, P50 and %HbF were negatively correlated (P<0.0001, r²=0.25). The clinical impact of %DRBCs was studied with the 6MWT. Q4 patients for the times <90% SpO2 and <88% SpO2 had higher %DRBCs than Q1 patients (P=0.03 and P=0.04, respectively). No between-group differences were observed for the times <90% SpO2 and <88% SpO2 for Hb or %HbF. Finally, in agreement with our previous demonstration that HU strongly decreased the %DRBCs >M6 of therapy and that the %DRBCs impacted the time at low SpO2, the 10 SCD patients' 6MWT results before and >M6 of HU therapy showed significantly decreased times <90% SpO2 (P=0.002) and <88% SpO2 (P=0.01) (Fig 2), and with delta SPO2 <4% (P=0.02). In conclusion, according to our results, the %DRBCs directly affects SCD patients' SpO2 during exercise; HU improves oxygen affinity in correlation with the %DRBC decline.
Under standard in vitro conditions (pH=7.4, pCO2 40 mm Hg, 37°C), the positions of oxyhemoglobin (A) dissociation curves of the different whole blood RBC fractions of an SS SCD patient and an AA control, and AA NDRBCs and SS DRBCs; (B) deoxygenation (–) and reoxygenation (- -) curves of the AA RBC fraction; (C) deoxygenation (–) and reoxygenation (- -) curves of the SS NDRBC fraction; (D) deoxygenation (–) and reoxygenation (- -) curves of the SS DRBC fraction.
Under standard in vitro conditions (pH=7.4, pCO2 40 mm Hg, 37°C), the positions of oxyhemoglobin (A) dissociation curves of the different whole blood RBC fractions of an SS SCD patient and an AA control, and AA NDRBCs and SS DRBCs; (B) deoxygenation (–) and reoxygenation (- -) curves of the AA RBC fraction; (C) deoxygenation (–) and reoxygenation (- -) curves of the SS NDRBC fraction; (D) deoxygenation (–) and reoxygenation (- -) curves of the SS DRBC fraction.
Comparison of times <90% SpO2, <88% SpO2 and with delta SpO2 >4% before and >M6 of HU.
Comparison of times <90% SpO2, <88% SpO2 and with delta SpO2 >4% before and >M6 of HU.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.