Abstract
Introduction:
B-cell lymphoma, unclassifiable(BCL-U) with features intermediate between diffuse large B-cell Lymphoma (DLBCL) and Burkitt Lymphoma (BL) shares some similarities with BL but has important genetic and clinical differences. These include older age at presentation for BCL-U and higher incidence of Bcl-2 over-expression. The outcomes and optimal treatment of BCL-U are not well defined. We reviewed the outcomes of patients with BCL-U and Burkitt lymphoma and analyzed the effect of treatment intensity.
Methods:
We performed a retrospective review of 92 consecutive patients diagnosed with BCL-U and BL receiving chemotherapy between 6/1994-11/2013 at the Case Comprehensive Cancer Center. Records were obtained from 59 patients treated at the Taussig Cancer Institute of the Cleveland Clinic and 35 patients at the Seidman Cancer Center of University Hospitals Case Medical Center. Chemotherapy regimens were categorized as intense (R-EPOCH, CODOX-M/IVAC, HyperCVAD) or less intense (R-CHOP, R-CVP, CHOP). Categorical variables were compared between groups using Fisher's exact test; all other variables were compared using the Wilcoxon rank sum test. Survival (OS) and progression-free survival (PFS) were calculated from the date treatment was started, using the Kaplan-Meier method. Comparison between groups was done using the log-rank test.
Results:
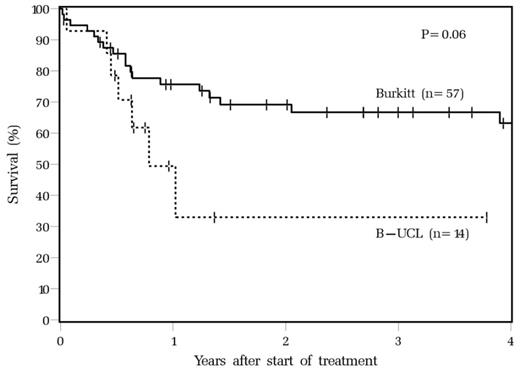
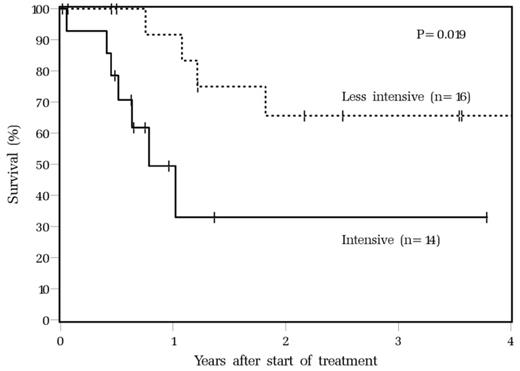
Sixty-two BL patients (67.4%) and 30 BCL-U (32.6%) patients were included. Patients with BCL-U were older (median age 54 vs. 48 in BL patients, p <0.001), with higher rates of Bcl-2 positivity by immunohistochemical (IHC) staining (66.7% vs. 7.5%, P<0.001). Myc translocation was present in 97% of BL patients vs. 65% of BCL-U (P=0.001). Among cases with known HIV status, 10 of 55 (18%) BL patients were HIV positive vs 1/24 (4.2%) for BCL-U (P=0.16). Other clinical characteristics including gender, ECOG performance status, stage, presence of B symptoms, and LDH levels were similar between the two groups. Fifty-seven BL (91.9%) and 14 BCL-U (46.7%) patients received intensive chemotherapy: CODOX-M/IVAC ± Rituximab (R), (BL=32; BCL-U =7), HyperCVAD ± R (BL=14; B-UCL=4), dose-adjusted EPOCH ± R (6 BL, 5 B-UCL) or other regimens (BL=8; BCL-U =2). R-CHOP was the most common less-intense regimen and was given to 4 patients with BL and 15 with BCL-U. Median follow-up was 39.5 months (range 0.4-110.7) in BL and 13.1 (0.2-62.1) in BCL-U. Consistent with previous reports, intensive therapy resulted in inferior outcomes for BCL-U than BL patients (3-year OS 33% vs. 66.8%, P = 0.06) (Figure 1). We also compared baseline characteristics of patients with BCL-U treated with intensive chemotherapy (N= 14) and those treated with less intense regimens (N = 16) and found that BCL-U patients treated with intensive therapy were significantly younger than those treated with less intense therapy (52 vs 72 years, P = 0.04), more likely to be male (85.7 vs.43.8%, P =0.017) and had more cases with Myc translocation (83.3% vs. 50%, P =0.11). There were 3 BCL-U patients treated with intensive therapy and 2 treated with less intensive therapy whose tumors harbored both Myc and Bcl-2 translocation (double-hit). Other demographic characteristics including stage, performance status and B–symptoms were comparable between two groups, as was the use of rituximab during initial treatment. BCL-U patients treated with less intensive regimens had superior 3-year OS compared with BCL-U subjects treated with intensive therapy (3 year OS 65.6% vs. 33%, p = 0.019) (Figure 2). All deaths except one among BCL-U patients were due to disease progression.
Overall survival of BL and B-UCL patients treated with intensive chemotherapy
Overall survival of B-UCL patients treated with intensive and less intensive chemotherapy.
Overall survival of B-UCL patients treated with intensive and less intensive chemotherapy.
Conclusions:
In this large dual-institution case series, we confirmed that intensive therapy for BCL-U results in inferior outcomes relative to BL. Somewhat surprisingly, less intensive treatment, more common in older BCL-U patients, was associated with improved OS relative to patients treated with intensive therapy. Biological differences in lymphoma, including a trend towards higher incidence of Myc translocations, as well as yet unknown patient factors may account for the poorer outcomes of BCL-U patients selected to undergo intensive therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.