Abstract
Background. The prognosis of patients with AL amyloidosis is mainly driven by the severity of heart involvement. Cardiac amyloidosis is being extensively studied, and accurate staging systems have been developed to identify patients with different degrees of heart dysfunction who are candidates for different treatment approaches. However, little is known on the outcome of patients without heart involvement who are generally considered low-risk. In the present study we evaluated factors affecting survival of patients with non-cardiac AL amyloidosis.
Patients and Methods. The subjects (n=135) without cardiac involvement (NT-proBNP <332 ng/L and mean left ventricular wall thickness at echocardiography £12 mm) and with normal troponin (Mayo Clinic stage I) were selected form the prospectively maintained database including 748 consecutive, previously untreated patients with AL amyloidosis diagnosed at our center between 2004 and 2012.
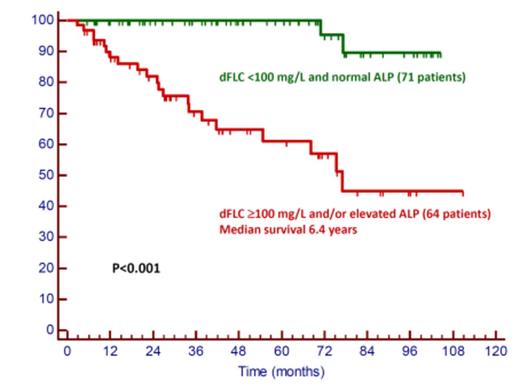
Results. Median age was 61 years (range 39-80 years). Involved organs were kidney (111, 82%); with median (range) proteinuria 7.2 g/24h (0.5-23.5 g/24h) and creatinine 1.1 mg/dL (0.5-4.4 mg/dL); soft tissues (21, 16%); liver (18, 13%), with median alkaline phosphatase (ALP) 2.3 times the upper reference limit (range 1.6-7.5 times u.r.l.); peripheral nervous system (13, 10%); gastrointestinal (GI) tract (10, 7%). One hundred seven patients (79%) had more than one organ involved. Median (range) bone marrow plasma cell infiltrate was 10% (2-29%) and dFLC (difference between involved and uninvolved free light chains) 70 mg/L (0-5721 mg/dL). Fifty-two patients (38%) were treated with melphalan / dexamethasone (MDex), 42 (31%) with bortezomib-based regimens, 14 (10%) underwent stem cell transplant (ASCT), 13 (10%) received thalidomide-based regimens, and the remaining patients received treatment for IgM clones or high-dose dexamethasone alone. After a median follow-up of living patients of 51 months, 23 patients (17%) died. Survival at 5 years was 82%. Twelve patients (52%) died a cardiac death (heart failure in 8 cases, sudden death in 4), after having developed cardiac involvement. All of them had baseline dFLC >100 mg/L. In these subjects the median NT-proBNP concentration at last assessment was 2401 ng/L, with a median 1646% increase compared to baseline. Of them 7 had failed to respond to frontline therapy, and the remaining had progressed after an initial partial response (PR, 3 cases) or very good partial response (VGPR, 2 cases). Eight patients (35%) died of liver failure. Six satisfied the criteria for liver involvement at baseline, and 2 developed hepatic amyloidosis during the follow-up, but had elevated ALP at baseline (1.3 and 1.4 times the u.r.l., respectively). Among them, 5 were non-responders to first-line therapy, and 3 had relapsed after PR (1) and VGPR (2). One patient died due to GI bleeding during ASCT. In the remaining 2 patients the causes of death were not directly related to the disease: myelodysplasia (5.9 years after having achieved VGPR with 6 cycles of MDex), and colorectal cancer (6.5 years after diagnosis). Only the two deaths that were not disease-related occurred in patients who presented with normal ALP and dFLC <100 mg/L (Figure). Elevated ALP (HR 5.11, P<0.001) and dFLC (HR 4.79, P<0.001) were independent prognostic factors at multivariate analysis.
Conclusion. This is the first study specifically addressing the outcome of patients with non-cardiac AL amyloidosis. Cardiac dysfunction after development of heart involvement remains the first cause of death also in patients who do not have cardiac involvement at diagnosis. Notably, fatal cardiac amyloidosis occurred only in patients in whom dFLC was >100 mg/L at diagnosis. Progressive liver involvement emerges as a significant cause of death in Stage I AL patients, and is predicted by elevated ALP. Patients with non-cardiac AL who have high dFLC and/or ALP should be treated aggressively to prevent the onset of terminal organ damage.
Merlini:Millennium Takeda: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.