Abstract
Introduction: We previously reported on the incidence of large granular lymphocytosis (LGL) following allogeneic hematopoietic cell transplantation (allo-HCT), its favorable impact on outcome and the predictive factors associated with its development (D Kim, BMT, 2013). In the current study we aimed to validate our previous findings in an independent set of patients.
Methods:All 408 patients undergoing allo-HCT at Princess Margaret Cancer Centre, Toronto, from 2007 to 2012 (replication set) were included retrospectively. Data from the previously reported set of patients undergoing allo-HCT from 2000 to 2007 (n = 418) (original set) were updated.
Results:There were significant differences between original and replication sets in baseline characteristics (age, underlying disease, conditioning, GvHD prophylaxis, graft source, donor type, and incidences of GvHD and CMV viremia) in accordance to the changes over a decade in allo-HCT procedures.
The cumulative incidence of LGL lymphocytosis at 3 years was 21.8% in the original set and 11.7% in the replication set (P<0.001). The median onset of LGL lymphocytosis was 362 days after HCT in the original set and 223 days in the replication set. Patients with LGL lymphocytosis showed a persistent elevation of lymphocyte count compared to patients without LGL lymphocytosis (P<0.001).
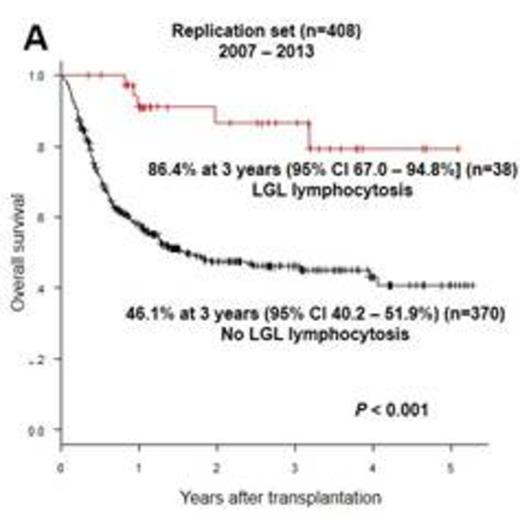
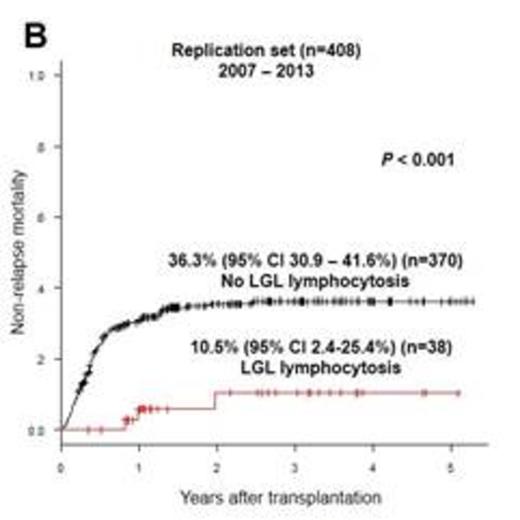
Patients with LGL lymphocytosis showed a higher overall survival (OS) (86.4% vs 46.1%, P<0.001, Fig. A) and lower non-relapse mortality (NRM) (10.5% vs 36.3%, P<0.001, Fig. B) at 3 years. No significant difference was found in relapse incidence according to the development of LGL lymphocytosis (13.9% vs 19.6%, P=0.25).
Multivariable analysis confirmed the favorable impact of LGL lymphocytosis on OS (HR 0.30, P=0.02) and a trend towards lower NRM (HR 0.27, P<0.001, original set; HR 0.50, P=0.22, replication set). No effect of LGL lymphocytosis on relapse incidence was demonstrated (HR 1.24, P=0.37, original set; HR 0.53, P=0.29, replication set).
Patients with LGL lymphocytosis showed a trend towards a higher incidence of IST cessation after cGvHD: 63.6% at 7 years vs 53.4% in patients without LGL lymphocytosis, P=0.07.
The previously identified predictive factors for the development of LGL lymphocytosis were replicated: higher incidence of LGL lymphocytosis with 1) CMV seropositive recipients (29.6% vs 5.1%, P < 0.001); 2) CMV viremia (31.0% vs 8.9%, P<0.001) and 3) chronic GvHD (28.2%, vs 5.0%, P<0.001).
Conclusions: The favorable impact of LGL lymphocytosis following allo-HCT in OS and NRM, as well as the predictive factors for the development of LGL lymphocytosis were successfully validated in an independent cohort of patients. No impact of LGL lymphocytosis on relapse incidence was noted. The difference in transplantation procedures between the two cohorts, such as GvHD prophylaxis/T-cell depletion, may explain the lower incidence of LGL lymphocytosis in the replication cohort. Patients with LGL lymphocytosis showed a trend towards a higher incidence of IST cessation after cGvHD, which may explain the lower NRM. Patients with LGL lymphocytosis showed a persistent elevation of lymphocyte count and had an indolent course.
OS and NRM according to the development of LGL lymphocytosis
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.