Abstract
Introduction
Nephrotic syndrome (NS) is characterized by massive proteinuria, hypoalbuminemia, and edema, and is associated with a complex acquired hypercoagulopathy and a high prevalence (~25%) of life-threatening thrombotic complications. However, anticoagulation is associated with a substantial risk for adverse bleeding events.
Recently published epidemiology studies suggest that proteinuria severity is directly correlated with thrombotic risk. However, further validation of this candidate biomarker for thrombotic risk requires appropriate validation and adequate pathophysiologic explanation. Results from recent experiments in our laboratory provide further evidence suggesting that proteinuria severity is directly proportional to hypercoagulability (as assessed by ex vivo and in vivo markers of thrombotic capacity) in two well-established animal models of NS (puromycin aminonucleoside (PAN) and Adriamycin (ADR) rats). Thus the aim of the present study was to further determine the relationship between proteinuria severity and endogenous thrombin potential (ETP), using a local cohort of prevalent and newly-diagnosed NS patients. We hypothesized that ETP is directly proportional to severity of proteinuria in human NS.
Methods
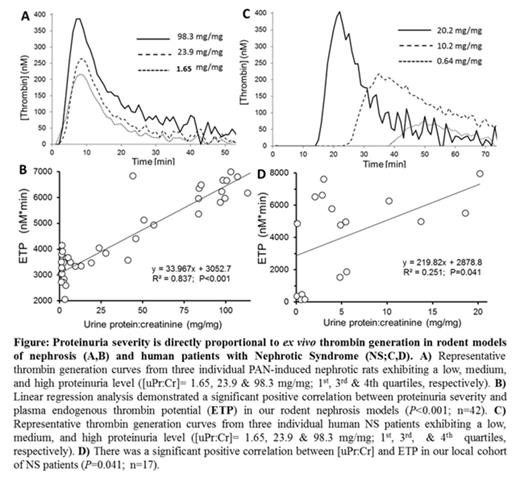
In order to fully examine proteinuria as a potential biomarker of thrombotic risk in NS, and to evaluate the usefulness of rodent NS models to study the NS-associated hypercoagulopathy, we first compared established markers of thrombin generation and global hemostasis in blood collected from the inferior vena cava (IVC) of male Wistar rats with PAN- or ADR- induced nephrosis (see above) exhibiting a range of proteinuria levels (morning spot urines analyzed for [protein:creatinine], uPr:Cr).
Pediatric and adult patients from Nationwide Children's Hospital and the Ohio State University's Wexner Medical Center who were not currently taking anticoagulant or antiplatelet agents and had no prior history of VTE were enrolled at the time of diagnosis with NS or during follow-up. Peripheral venous blood from these patients (6 children and 11 adults) was collected into 0.32% NaCitrate/1.45 µM Corn Trypsin Inhibitor [final concentrations] and immediately spun down to platelet poor plasma (PPP). Thrombin generation assays (TGA) were then performed and ETP correlated to corresponding spot urines analyzed for uPr:Cr, as obtained from clinical lab records. This study was approved by the Nationwide Children's Hospital IRB, which has a reciprocity agreement with the OSUWMC IRB.
Results
When the final results from our experimental animal model studies were merged, the combined TGA data from both PAN and ADR models of NS revealed a significant positive correlation between proteinuria severity and thrombin generation (ETP; R2=0.837, P<0.001; Fig A&B). Thus, we sought to determine if this relationship was also present in human patients with NS. As expected, our local cohort of prevalent and newly-diagnosed NS patients exhibited a range of proteinuria values (median (range): 3.93 mg/mg (0.11-20.2)). Importantly, analysis of thrombin generation in these NS patients demonstrated that proteinuria severity was directly proportional to hypercoagulability (Fig C), such that there was a significant positive correlation between Ur Pr:Cr and ETP (R2=0.251, P=0.041; Fig D).
In contrast, although plasma albumin levels were significantly negatively correlated with ETP in our rodent models (R2=0.852, P<0.001), we found no correlation between serum albumin and ETP in our human patient cohort (R2=0.062, P=0.314).
Conclusions
These data confirm that proteinuria severity in both rodents and humans with NS is directly proportional to ETP, an established marker of thrombin generation that is known to correlate with thrombotic risk. Taken together, these data strongly suggest that proteinuria severity is a promising biomarker for thrombotic risk in NS, and that it may be superior to serum albumin. Animal models of NS may provide outstanding opportunities to further define the molecular pathophysiology by which proteinuria enhances thrombin generation and clinical risk for thrombosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.