Abstract

Introduction: Survivors of Thrombotic Thrombocytopenic Purpura (TTP) hospitalizations have been proposed to be at higher risk for long term poor clinical outcomes and premature death. Patients with TTP have a high risk for in-hospital morbidity and mortality as well. However, there is a paucity of data on the predictors of adverse outcomes including death in hospitalized patients with TTP.
Methods: A weighted analysis of 5 years (2007-2011) using data from the Nationwide Inpatient Sample, a stratified probability sample of 20% of all hospital discharges among community hospitals in the United States (approximately 1100 hospitals/year), was performed. Hospitalizations with TTP as the primary admitting diagnoses were identified using the ICD-9 discharge code 446.6. Univariate and stepwise multivariable logistic regression analyses with elimination were used for statistical analysis. Based on results of univariate analysis, the significant variables were added in a stepwise manner in a multivariable model. All variables selected for the multivariable model were tested for interaction with a significance threshold level of p<0.2. Except for this, all hypothesis testing was two tailed and p<0.05 was considered significant. Receiver Operator Characteristics (ROC) curve was constructed using risk factors on multivariate analysis.
Results: The all-cause mortality rate was 8.7% (918/10615) among admissions with primary diagnosis of TTP (0.5% pediatric, 65.9% female, 58.2% Caucasian, 27.2% African-American). Table 1 lists the risk factors by univariate analysis and includes a) factors with significantly higher odds of mortality and b) other putative factors which were not statistically significant predictors.
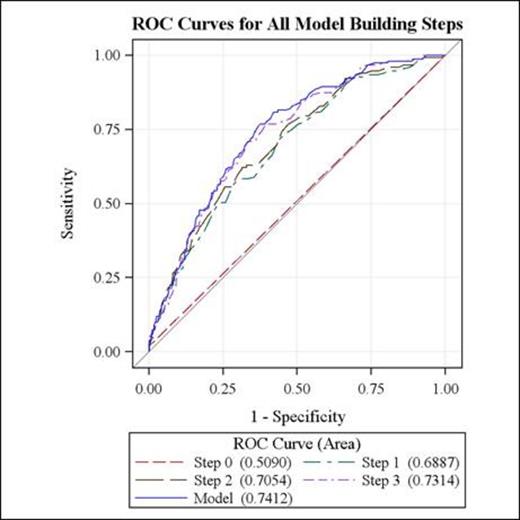
Table 2: In stepwise multivariable logistic regression analysis: arterial thrombosis (adjOR 5.1 95%CI=1.1-31.7), acute myocardial infarction (adjOR 2.8, 95%CI=1.6-4.9), non-occurrence of either intervention: plasmapheresis or fresh frozen plasma infusion (adjOR 2.0, 95% CI=1.4-2.9) 4) requirement of platelet transfusions during hospitalization (adjOR 2.0, 95%CI= 1.3-3.2) and every ten year increase in age (OR 1.4 95%CI=1.3-1.6) were independently predictive of mortality in TTP patients (area under the curve for ROC 74%, Figure 1).
Conclusion: We present a set of independent risk factors that may potentially be used in a predictive model of mortality in TTP. Early and targeted aggressive therapy based on these factors should guide the management of hospitalized patients with TTP for improved outcomes.
Unadjusted odds of in-hospital mortality.
| Significant predictors of mortality for TTP on univariate analysis . | Odds Ratio . | 95% Confidence Limits . | |
|---|---|---|---|
| Arterial Thrombosis | 10.9 | 2.2 | 54.6 |
| AMI | 3.7 | 2.1 | 6.2 |
| STROKE | 4.9 | 3.0 | 7.9 |
| Platelet Transfusion | 2.3 | 1.5 | 3.6 |
| Bleeding event | 1.7 | 1.1 | 2.6 |
| Plasmapheresis (No vs. Yes) | 1.6 | 1.2 | 2.3 |
| plasmapheresis or plasma infusion (not performed) | 2.2 | 1.5 | 3.1 |
| Every 10 years increase in age | 1.5 | 1.3 | 1.6 |
| PRBC transfusion | 1.7 | 1.2 | 2.3 |
| Caucasian versus African American | 1.9 | 1.3 | 2.8 |
| Asian versus African American | 3.3 | 1.2 | 9.1 |
| V ariables not significant predictors of mortality for TTP on univariate analysis. | Odds Ratio | 95% Confidence Limits | |
| Venous Thrombosis/Thromboembolism | 1.9 | 0.8 | 4.4 |
| FEMALE versus male gender | 1.0 | 0.7 | 1.4 |
| Hypertension Yes vs. no | 0.9 | 0.6 | 1.2 |
| Diabetes Yes vs. no | 0.9 | 0.6 | 1.4 |
| Chronic Kidney Disease Yes vs. No | 1.4 | 0.9 | 2.2 |
| End Stage Renal Disease Yes vs. No | 0.9 | 0.4 | 1.9 |
| Overweight/Obese Yes vs. No | 0.7 | 0.4 | 1.5 |
| Variables meeting criteria for inclusion in multiple logistic regression model are in boldface type. | |||
| Significant predictors of mortality for TTP on univariate analysis . | Odds Ratio . | 95% Confidence Limits . | |
|---|---|---|---|
| Arterial Thrombosis | 10.9 | 2.2 | 54.6 |
| AMI | 3.7 | 2.1 | 6.2 |
| STROKE | 4.9 | 3.0 | 7.9 |
| Platelet Transfusion | 2.3 | 1.5 | 3.6 |
| Bleeding event | 1.7 | 1.1 | 2.6 |
| Plasmapheresis (No vs. Yes) | 1.6 | 1.2 | 2.3 |
| plasmapheresis or plasma infusion (not performed) | 2.2 | 1.5 | 3.1 |
| Every 10 years increase in age | 1.5 | 1.3 | 1.6 |
| PRBC transfusion | 1.7 | 1.2 | 2.3 |
| Caucasian versus African American | 1.9 | 1.3 | 2.8 |
| Asian versus African American | 3.3 | 1.2 | 9.1 |
| V ariables not significant predictors of mortality for TTP on univariate analysis. | Odds Ratio | 95% Confidence Limits | |
| Venous Thrombosis/Thromboembolism | 1.9 | 0.8 | 4.4 |
| FEMALE versus male gender | 1.0 | 0.7 | 1.4 |
| Hypertension Yes vs. no | 0.9 | 0.6 | 1.2 |
| Diabetes Yes vs. no | 0.9 | 0.6 | 1.4 |
| Chronic Kidney Disease Yes vs. No | 1.4 | 0.9 | 2.2 |
| End Stage Renal Disease Yes vs. No | 0.9 | 0.4 | 1.9 |
| Overweight/Obese Yes vs. No | 0.7 | 0.4 | 1.5 |
| Variables meeting criteria for inclusion in multiple logistic regression model are in boldface type. | |||
Multivariable Predictors for In Hospital Mortality in patients with primary diagnosis of TTP
| . | Adjusted Odds Ratio . | 95% Confidence Limits . | |
|---|---|---|---|
| Arterial Thrombosis | 6.0 | 1.2 | 30.5 |
| Acute myocardial infarction | 2.8 | 1.6 | 4.8 |
| No Plasmapheresis/Plasma infusion | 2.0 | 1.4 | 2.9 |
| Platelet Transfusion | 2.1 | 1.4 | 3.2 |
| Age (per 10 year higher) | 1.4 | 1.3 | 1.6 |
| Female versus Male | 1.2 | 0.8 | 1.7 |
| TTP = Thrombotic Thrombocytopenic Purpura | |||
| . | Adjusted Odds Ratio . | 95% Confidence Limits . | |
|---|---|---|---|
| Arterial Thrombosis | 6.0 | 1.2 | 30.5 |
| Acute myocardial infarction | 2.8 | 1.6 | 4.8 |
| No Plasmapheresis/Plasma infusion | 2.0 | 1.4 | 2.9 |
| Platelet Transfusion | 2.1 | 1.4 | 3.2 |
| Age (per 10 year higher) | 1.4 | 1.3 | 1.6 |
| Female versus Male | 1.2 | 0.8 | 1.7 |
| TTP = Thrombotic Thrombocytopenic Purpura | |||
Step 0: Using arterial thrombosis
Receiver- Operator-Characteristic Curve (ROC) overlay curve for the stepwise multivariable logistic regression risk prediction showing incremental AUC with addition of each risk factor for hospital patients with TTP.
Receiver- Operator-Characteristic Curve (ROC) overlay curve for the stepwise multivariable logistic regression risk prediction showing incremental AUC with addition of each risk factor for hospital patients with TTP.
Step 1: Adding acute myocardial infarction
Step 2: Adding plasmapheresis /fresh frozen plasma infusion
Step 3: Adding platelet transfusions
Final model: Adding every ten year increase in age.
Ness:Terumo BCT: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract