Abstract
Background: Burkitt lymphoma typically involves the bone marrow in advanced stage disease. Pure leukemic presentation of Burkitt lymphoma (pure Burkitt leukemia) with negative radiographic findings is uncommon but considered clinically as stage IV disease. The WHO classification clearly distinguishes Burkitt leukemia (formerly classified as FAB-L3) from B lymphoblastic leukemia, as the former has a mature B-cell phenotype (expresses surface immunoglobulin) and characteristically harbors a MYC translocation with an immunoglobulin partner. There is limited prognostic information on patients with pure Burkitt leukemia (PBL) because they are typically combined with Burkitt lymphoma patients with widespread disease (WBL).
Methods: We performed a multicenter retrospective analysis of newly-diagnosed Burkitt lymphoma cases involving the bone marrow at four academic medical centers from 2000-2013. Inclusion criteria included availability of clinical information and follow-up data, MYC rearrangement, and treatment with intensive chemotherapy (Hyper-CVAD or ALL-like regimens). Pediatric patients were excluded (age < 21 years). Diagnosis was established by the institutions' expert hematopathologist in conjunction with cytogenetic, flow cytometric, and radiographic findings. Patients were placed in the pure Burkitt leukemia (PBL) group if they had bone marrow involvement but were otherwise radiographically negative (i.e. PET negative). Kaplan-Meier analysis was used to examine the difference in overall survival between the WBL and PBL groups. We also determined prognostic factors associated with survival in univariate and multivariate Cox regression analyses.
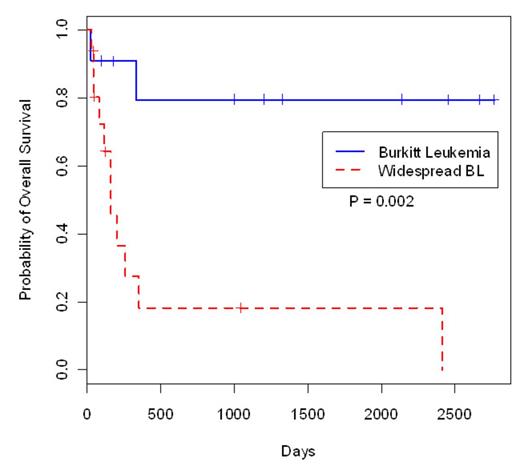
Results: We identified 51 patients with bone marrow involvement by Burkitt lymphoma. Of these patients, 24 were excluded because of a lack of clinical or follow-up information (15), pediatric age group (7), no treatment initiated (1), or misdiagnosed and given inadequate treatment (1). Of the 27 patients that met our inclusion criteria, 11 patients had pure Burkitt leukemia (PBL) and 16 had tissue involvement with bone marrow disease (WBL). The male-to-female ratio in the PBL group was 4.5:1 and in the WBL 4:1 (p=0.23). The median age for the PBL was 46 years vs 47 years in the WBL (p=0.34). CSF involvement was similar in both groups (30% PBL vs. 38.5% WBL; p=0.14); with elevated LDH levels in all patients in both groups (PBL median 3399 IU/L, WBL 2550 IU/L; p=0.81). In general, the WBL group had more complex karyotypes and a significantly greater number of cases with chromosome 1q abnormalities (5/7, 71%) compared to the PBL group (1/5, 20%). In the survival analysis, patients with PBL exhibited significantly better survival with a 5-year-overall survival of 79.5% (95% CI: 57.7-100%) vs. 18.4% (95% CI: 5.3-63.3%) in the WBL group (p=0.002).
Conclusion: To the best of our knowledge, this is the largest series comparing adults with pure Burkitt leukemia and Burkitt lymphoma with widespread disease. Within the limitations of a retrospective analysis, the 5-year overall survival for the widespread Burkitt lymphoma (WBL) group is inferior compared to pure Burkitt leukemia (PBL) treated with intensive chemotherapy. Interestingly, the WBL group had more complex karyotypes compared to the PBL group.
Overall Survival of Burkitt Leukemia versus Widespread Burkitt Lymphoma (BL).
Overall Survival of Burkitt Leukemia versus Widespread Burkitt Lymphoma (BL).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.