Abstract
Background
Chronic myelomonocytic leukemia (CMML) is a rare hematological malignancy with features of both myelodysplastic syndromes (MDS) and myeloproliferative neoplasms. Most data on CMML arrive from the few available clinical and epidemiological studies where CMML was often combined with MDS. So far, phase 3 clinical trials and large population-based studies specifically addressing CMML are lacking. We conducted a large nationwide population-based study to assess trends in incidence, primary treatment and survival among CMML patients in the Netherlands from 1989-2012.
Methods
We selected all patients diagnosed with CMML in 1989-2012 (N = 1,359; median age 75 years; age range 22-95 years; 63% males) from the nationwide population-based Netherlands Cancer Registry (NCR). Patients with juvenile myelomonocytic leukemia were excluded. Despite changes in classification, separate morphology codes for CMML were available in all editions of the International Classification of Diseases for Oncology (ICD-O; 9893, 9868 and 9945 in the first, second and third edition, respectively) and could therefore be identified in the NCR throughout the whole study period. The ICD-O does not have separate codes for CMML-1 or 2. Data on primary treatment, that is, no therapy or only supportive care (NT/SC), chemotherapy (CT) and CT followed by a stem cell transplantation (CT + SCT), were retrieved from the NCR. Patients were categorized into three calendar periods (1989-2000, 2001-2006 and 2007-2012) and four age groups (18-59, 60-69, 70-79 and ≥80 years), unless otherwise stated. Incidence rates were age-standardized to the European standard population and calculated per 100,000 person-years. Relative survival rates (RSRs) were computed as a measure of disease-specific survival.
Results
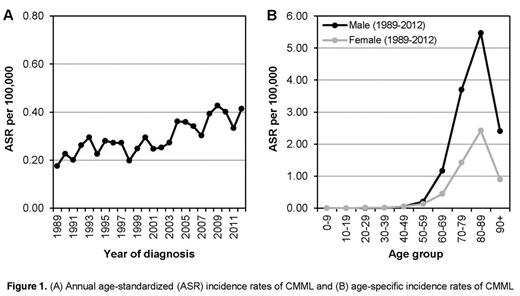
The overall age-standardized incidence rate (ASR) of CMML increased from 0.23 per 100,000 in 1989-2000, 0.31 in 2001-2006 to 0.38 in 2007-2012. The annual ASR became stable at around 0.4 per 100,000 since 2008 (Fig 1A). The proportion of patients diagnosed in individuals aged ≥70 years was 70%. The incidence of CMML was higher in men than in women, which was ascribed to the higher incidence among the 70-year-old men compared with the equivalent female group (Fig 1B).
The primary treatment of CMML patients remained unchanged during the entire study period. In the overall series, 975 (72%), 365 (27%) and 19 (1%) CMML patients received NT/SC, CT and CT + SCT, respectively. The use of CT + SCT was mainly restricted to patients 18-59 (n = 13) and 60-69 (n = 6) years of age.
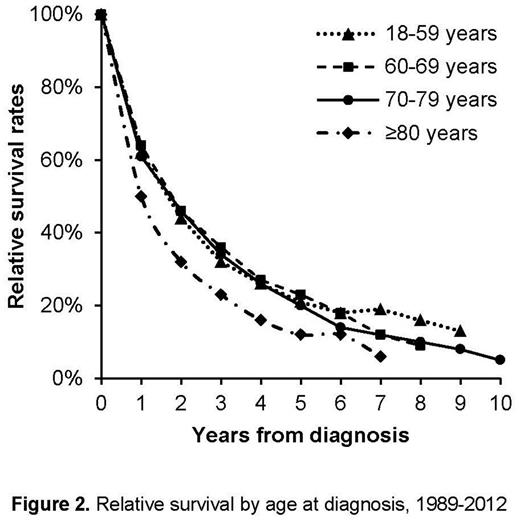
Survival of CMML patients was poor and did not improve over time as the 5-year RSRs (with 95% confidence interval) were 16% (12%-20%), 20% (15%-25%) and 20% (15%-25%) in the three calendar periods, respectively. As shown in Figure 2 , the overall 5-year RSRs for patients in the four age groups were 21% (13%-29%), 23% (18%-29%), 20% (16%-24%) and 12% (7%-18%), respectively. With the limitation of small numbers (n = 19), the overall 5- and 10-year RSRs were 29% (10%-52%) and 30% (10%-53%) for patients undergoing CT + SCT as primary treatment. In other words, the RSR reached a plateau after 5 years since diagnosis. In the most recent period, the 5-year RSR was 73% (25%-95%) for patients undergoing CT + SCT (n = 7).
Conclusions
In this first large population-based study including almost 1400 CMML patients, we found that the incidence of CMML increased over time until the year 2007. This rise is probably explained by improved case ascertainment and augmented disease awareness, rather than by changes in etiologic factors. Primary treatment remained conservative throughout the study period as treatment options for CMML, which primarily affects the elderly, are very limited. As a consequence, relative survival remained poor and essentially unchanged in both younger and older patients over the past two decades. Therefore, CMML-specific prognostic models should be applied in the diagnostic work-up to evaluate prognosis and plan risk-adapted treatment, and assist in designing clinical trials that specifically assess therapeutic options in CMML patients in order to improve their survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.