Abstract
Background: Multiple myeloma (MM) is characterised by the production of monoclonal immunoglobulin (Ig) and clonal proliferation of neoplastic plasma cells in bone marrow. The emergence of oligoclonal bands (OB) in serum and/or urine immunofixation electrophoresis (IFE) that is different to that observed at diagnosis has been reported with varying frequency in patients with stem cell transplantation (SCT) or favourable response to chemotherapy, although its prognostic relevance remains unclear. Here, we retrospectively analysed clinical records and results serial serum and/or urine IFE to determine the frequency, clinical characteristics and prognostic impact of OB that developed after treatment. We also analysed the effects of OB on the results of free light chain (FLC) assay that may affect the stringent CR (sCR) criteria proposed by the IMWG.
Patients: We retrospectively reviewed 180 patients with MM admitted to the Department of Hematology/Oncology at Kameda Medical Center, Kamogawa, Japan, from January 2006 to May 2014.Seventeen patients were excluded from the analysis due to lack of appropriate follow-up data.
Method: An OB was defined as the presence of a serum and/or urine IFE monoclonal spike that was different from the original myeloma protein in heavy and/or light chains, as well as a different IFE migration pattern. IFE was performed at least every three months after obtaining very good partial response (VGPR) and then until the disease progression or relapse was confirmed. Overall survival (OS) and progression free survival (PFS) were analyzed in 173 MM patients by the Kaplan–Meier method, and differences between the curves were calculated by two-sided log-rank test. Free light chain (FLC) and minimal residual disease measurement by multicolour flowcytometory (MFC) were performed to evaluate the response to treatment.
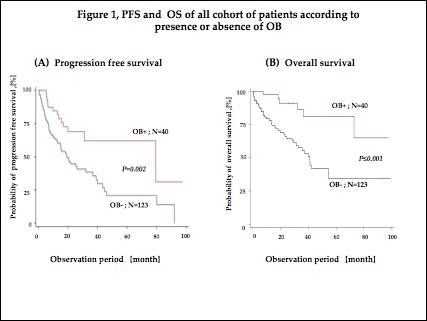
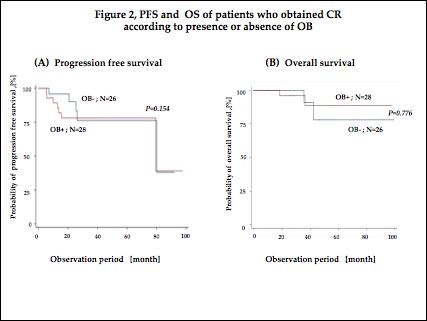
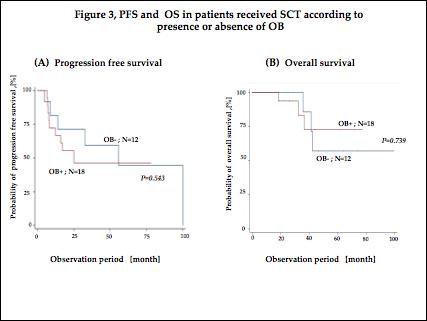
Results: Myeloma response more than VGPR and CR were achieved in 87 (53.3%) and 54 (33.1%) patients, respectively. None of the patients with less than PR developed OB, and OB developed in 36.3% (12/33) and 51.9% (28/54) of the patients with VGPR and CR, respectively. Among the 30 patients who received SCT, 18 patients (60.0%) developed OB, whereas only 12 of 133 patients who did not receive SCT developed OB. The emergence of OB was significantly higher in patients receiving SCT (P < 0.001). The median PFS of the patients with and without OB were 79.4 months and 19.2 months (P = 0.028), respectively, and those of OS did not reached and 41.1 months (P < 0.001), respectively (Figure 1). However, if patient response was limited to CR, median PFS and OS of patients with and without OB were not significantly different between the two groups (79.4 months vs. 80.1months, respectively, P = 0.646; and not reached and not reached, respectively, P = 0.776; Figure 2). OB was observed in 60% of patients after SCT, and in 36.6% of patients more than VGPR without SCT (P<0.001). In the patients who received SCT, the presence of OB was not associated with either PFS or OS (20.0 months vs 44.7 months, P=0.543 and not reached vs not reached, P= 0.739, respectively; Figure3). We also analyzed the association between residual myeloma cells assessed by the MFC in the patients who achieved CR according to the development of OB. Although the patients with OB showed slightly lower levels of residual myeloma cells than those without OB (2.49 x10-4vs 4.15 x10-4), there was no significant difference between the two groups (P= 0.054). As the presence of OB may result in an abnormal serum FLC kappa/lambda ratio, we examined the association of FLC kappa/lambda ratio and development of OB in 28 patients who achieved CR. Abnormal FLC kappa/lambda ratio was observed in 10 (35.7%) and 4 (15.3%) patients with and without OB, respectively, among those with CR (P = 0.118). Conversely, OB was detected in 10 of the 14 patients with an abnormal FLC ratio (71.4%) versus 18 of 40 (45.0%) with a normal serum FLC ratio (P = 0.164) among those with CR.
Conclusions: In conclusion, we showed that the emergence of OB occurred exclusively in patients with favourable myeloma responses (more than VGPR) and was associated with prolonged survival. Patients with OB appeared to have fewer residual myeloma cells compared to those without OB. However, its development did not confer an additional survival benefit among the patients who achieved CR. In addition, it is possible that the emergence of OB affects the sCR response criteria proposed by the IMWG.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.