Abstract
Background: There are no prospective studies comparing the effectiveness of the three iron chelators commercially available in preventing or decreasing iron overload in the heart and liver in pediatric thalassemia major (TM) patients. Our aim was to evaluate the changes in cardiac and hepatic iron and in cardiac function by quantitative magnetic resonance imaging (MRI) over a follow-up (FU) of 18 months in pediatric TM patients treated with one of the 3 available iron chelators in monotherapy or non chelated.
Methods: Among the first 1611 TM patients enrolled in the MIOT (Myocardial Iron Overload in Thalassemia) network, we considered pediatric patients who had maintained the same chelation regimen between the two MRI scans. Iron overload was quantified by multiecho T2* sequence. Hepatic T2* values were converted into liver iron concentration (LIC) values. Biventricular function parameters were evaluated by cine images. Due to the low sample size, no inter-treatment comparisons were performed and intra-treatment comparison was performed only in the DFX group.
Results: Four groups of patients were identified: 6 patients (3 F, 10.0±2.2 years) treated with desferioxamine (DFO– mean dosage 43.7±6.8 mg/kg/die), 7 patients (3 F, 15.5±1.7 yrs) treated with deferiprone (DFP– mean dosage 75.0±9.2 mg/kg/die), 39 patients (13 F, 13.58±3.39 yrs) treated with deferasirox (DFX– mean dosage 26.6±6.7 mg/kg/die), and 2 patients (2 F, 11.1±5.3 yrs) not chelated because they had performed a bone marrow transplantation. Compliance to chelation therapy was excellent/good in all treated groups.
At baseline in DFO, DFP and no chelated groups no patient showed a global heart T2* value<20 ms. In all 4 groups all patients who showed no cardiac iron overload at baseline maintained at the FU the same status. At baseline in DFX group 6 patients (17.6%) had heart T2* values<20 ms. The 4 patients with intermediate cardiac iron (T2* 10-20 ms) at the baseline showed no iron at the FU while the patient with severe cardiac iron (T2*<10 ms) remained in the same status at the FU. Non chelated patients had higher global heart T2* values at baseline (non-chelated 37.7±0.5 ms > DFP 35.3±4.9 ms > DFX 32.7±9.6 ms > DFO 31.9±10.5 ms) while DFP patients had higher global heart T2* values at FU (DFP 39.5±6.1 ms > DFX 34.2±7.3 ms > DFO 33.6±7.9 ms > non-chelated 28.9±4.0 ms ).
In the DFO group at baseline 1 patient showed pathological left ventricular ejection fraction (LVEF) and he recovered at the follow up. In the DFP group at baseline 2 patients showed pathological LVEF and both recovered at the follow up. In the DFX group at baseline 3 patients showed pathological LVEF: 2 recovered at the FU and 1 did not perform the evaluation of the cardiac function at FU due to technical reasons. Conversely 9 patients with normal LVEF at baseline showed pathological LVEF at the FU.
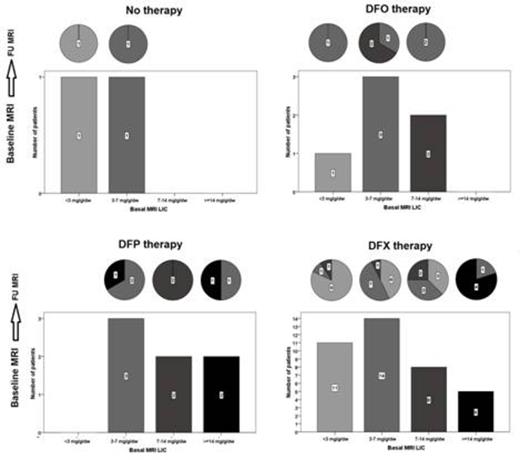
In the DFO group the percentage of patients with MRI LIC>3 mg/g/dw went up from 83% to 100%. In the DFP group all patients showed MRI LIC>3 mg/g/dw at baseline and they maintained this status at the FU. In the DFX group the percentage of patients with MRI LIC≥3 mg/g/dw went down from 71.1% to 52.6%. The MRI LIC mean difference was -1.6±4.4 mg/g/dw (P=0.006). Only one of the two non chelated patients had a baseline MRI LIC≥3 mg/g/dw and she remained in the same status at the FU.
Conclusion: This longitudinal analysis confirms significant rate of iron overload even in very young TM population, in particular in the liver. In this population, DFP seems to be more effective in the heart with a concordant positive effect on the global systolic function. Conversely, DFX seems to be more effective in the liver. However, further prospective studies are needed on larger study population to confirm the data.
Pepe:Chiesi: Speakers Bureau; ApoPharma Inc.: Speakers Bureau; Novartis: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.