Abstract
Background: The Glasgow Prognostic Score (GPS), consisting of C-reactive protein (CRP) and albumin (Alb), is clinically useful for tumor behavior and shows significant prognostic value in several types of tumors. Several studies showed that GPS could be a predictive marker for advanced solid tumor, such as colorectal cancer, gastric cancer, etc. Now we performed a retrospective study to evaluate the relationship between GPS and prognosis of 160 patients with diffuse large B cell lymphoma (DLBCL) receiving R-CHOP chemotherapy between January 2001 and May 2010 at Shanghai Ruijin Hospital.
Methods: Before treatment, the CRP and albumin were both tested for base line. Patients with both elevated CRP level (>10 mg/L) and hypoalbuminemia (<35 g/L) were given a score of 2. Patients with only one of these two biochemical abnormalities were allocated a score of 1. Patients in whom neither of these abnormalities was presented received a score of 0. We also identified International Prognostic Index (IPI) score of these patients.
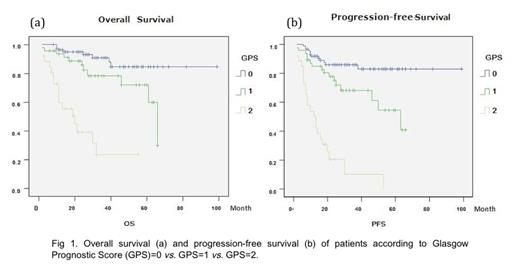
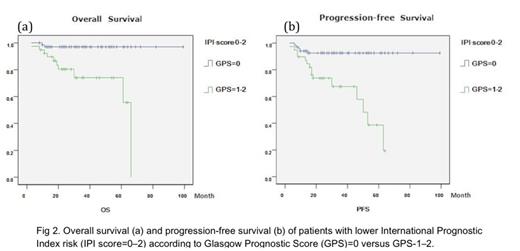
Results: Patients were assorted into three groups based on GPS at diagnosis. Survival curves were performed using the Kaplan-Meier method. Results showed that the overall survival (OS) and progress-free survival (PFS) rates for all patients were 78.1% and 68.1%, respectively. Analyzed by log-rank test, there was significant difference between GPS 1, GPS 2 and GPS 3 for OS (90.8% vs. 76.6% vs. 38.5%, p<0.001) and PFS (86.2% vs. 66.0% vs. 15.4%, p<0.001) (Fig 1a and b). In addition, the IPI, as a well-accepted prognostic system, though showed significant difference between lower risk group (IPI 0-2) and higher risk group (IPI 3--5) for OS (89.1% vs. 54.0%, p<0.01), failed to identify patients with poor prognosis in the lower risk group, since the low risk (IPI=0-1) and low-intermediate risk groups (IPI=2) appeared closely overlapping (p>0.05). While combining with the IPI model, GPS can have powerful prognostic value in the lower-risk (IPI=0-2) DLBCL patients, since patients with GPS score=0 had better OS (P<0.001) and PFS (P<0.001) than those with GPS score=1--2(Fig 2a and b).
Conclusion: The GPS was a reliable and independent predictor of OS and PFS in patients with DLBCL treated with R-CHOP regimen. GPS combining with the IPI score may offer a more integrated prognostic system in the rituximab era of DLBCL. And inflammatory response might play an important role in the progression and survival of patients with DLBCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.