Abstract
Background:
Extranodal natural killer T (NK/T) -cell lymphoma, nasal-type, is a recognized entity within the WHO classification of lymphoid tumors. This neoplasm is a rare, and is well documented in East Asia. It is not commonly seen in the United States; however the overall prevalence and incidence of this lymphoma has started to increase. Due to its rare prevalence in the United States, a standardized chemotherapy regimen and a prognostic model have yet to be established in patients diagnosed with this lymphoma.
Methods:
In this retrospective study, we reviewed a total of 25 patients with a diagnosis of extranodal NK T cell lymphomas nasal type. Several variables were assessed including international prognostic index (IPI), performance status, regional lymph node involvement, bone marrow involvement, and proliferation index (high proliferation index defined as Ki67/MIB expression in > 50% cells). We assessed the clinical outcome using various treatment modalities over the last 2 decades.
Results
The majority of the patients in this study were males 20 (80%). The median age of patients was 46 (20-72), and most patients were Hispanic (80%). Ann Arbor staging was performed and was noted as follows: stage I (12), stage II (5), stage III (3), and stage IV (5). Patient were risk stratified into IPI score and ECOG PS score: IPI score < 2 (17), IPI > 2 (8), ECOG < 2 (19) and ECOG >2 (6). Nine patients were treated with RCHOP + radiation (XRT) and 10 patients were treated with hyper CVAD therapy + XRT. Seven patients were treated with a non-anthracycline based approach: VIPD+ XRT (2), DEVIC + XRT (3), and SMILE+ XRT (2).
The five year overall survival of this group was 38.4%. An IPI score > 2 was noted to have significant poor prognosis with a median survival of 15 months in comparison to 22 months (p< 0.001) for IPI < 2. Bulky cervical lymphadenopathy and bone marrow involvement at diagnosis were poor prognostic indicators of overall survival. Patients who presented with bulky cervical lymphadenopathy or evidence of bone marrow involvement at diagnosis were noted to have a median survival time of 12 months, as compared to no involvement had a median survival of 22 months ( p<0.001). A high proliferation index was also associated with a poor prognosis as well. Patients who were noted to have a high proliferation index had a median survival of 15 months as compared to 22 months in patients who were noted to have a low proliferation index (p< 0.001).
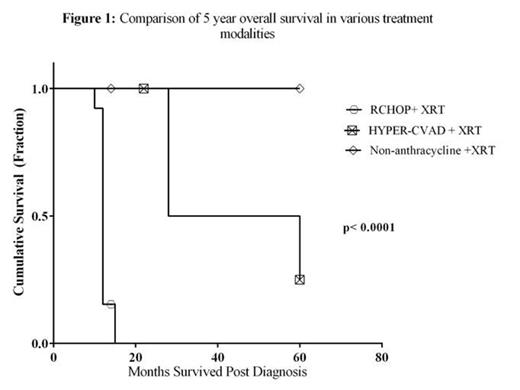
Median survival in patients treated with RCHOP + XRT was noted be 12 months in comparison to patients with HYPER-CVAD+ XRT (24 months) and non-anthracycline approach (28 months) (p< 0.001). In addition, patients treated with RCHOP +XRT were noted to have increased incidence of disease progression comparison to patients treated with HYPERCVAD+ XRT and non-anthracycline based therapy +XRT (p< 0.0001) (Figure 1).
Conclusions:
In this retrospective analysis, we demonstrated that extra-nodal NK T cell, nasal type has a poor prognosis. Preliminary data from this study suggests hyperCVAD or a non-anthracycline based chemotherapy approach with concomitant radiation are superior to RCHOP with concomitant radiation. The results of this study also provided promising results for a prognostic model against this lymphoma in the future. These results underscore the need for further investigation for this lymphoma in the future.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.