Abstract
Background:
AYA (15-39y) diagnosed with hematologic malignancies have inferior survival and have not seen the same survival improvement in comparison with those diagnosed during childhood (0-14y) leaving an AYA Gap. Treatment on pediatric trials is associated with superior survival in 15-21y diagnosed with acute lymphoblastic leukemia (ALL). However, impact of care at National Cancer Institute-designated Comprehensive Cancer Centers (NCICCC) for AYA of all ages or Children’s Oncology Group sites (COG) for AYA aged 15-21y remains unstudied.
Methods:
We constructed a population-based cohort of 1,388 children (1-14y), 673 young AYA (15-21y) and 2,275 older AYA (22-39y) with newly diagnosed ALL, acute myeloid leukemia (AML), Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) reported to the LA County cancer registry between 1998-2008. We sought to determine the impact of care at NCICCC/COG (NCICCC+COG: n=3, COG: n=3) on overall survival (OS) and barriers to access to care at NCICCC/COG in AYA with hematologic malignancies. Multivariable Cox regression was used to derive hazard ratios (HR) for mortality, adjusting for gender, race/ethnicity, socioeconomic status (SES) [and stage in lymphomas]. Multivariable logistic regression was used to derive odds ratios (OR) for likelihood of care at NCICCC/COG, adjusting for above variables plus insurance and distance to the nearest NCICCC/COG. Distance to NCICCC/COG was derived using Geographic Information Systems.
Results:
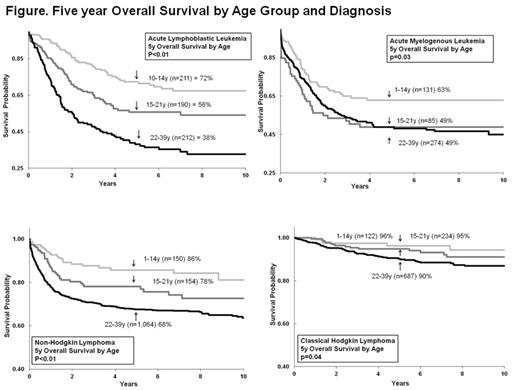
AYA experienced inferior 5y OS as compared to children across diagnoses (Figure: ALL [n=1,380]: 72% [10-14y] vs 44% [15-21y] vs 38% [22-39y], p<0.01; AML [n=490]: 63% [1-14y] vs 49% [15-21y] vs 49% [22-39y], p<0.01; NHL [n=1,379] : 86% [1-14y] vs 78% [15-21y] vs 68% [22-39y], p<0.01; HL [n=1,087]: 96% [1-14y] vs 95% [15-21y] vs 90% [22-39y], p=0.04). AYA with ALL treated at community sites had worse outcome when compared with children (15-21y vs 10-14y: HR=2.9, p<0.01; 22-39y vs 10-14y: HR=4.7, p<0.01). This difference in outcome between young AYA and children with ALL was abrogated by care at NCICCC/COG (HR=1.3, p=0.2) and greatly diminished in older AYA by care at NCICCC (HR=2.5, p<0.01). Similarly, AYA with AML treated at community sites had worse outcome when compared with children (15-21y vs 1-14y: HR=2.3, p<0.01; 22-39y vs 1-14y: 1.8, p=0.07). The difference in outcome was abrogated by care at NCICCC/COG (young AYA vs children with AML: HR=1.1, p=0.07; older AYA vs children: HR=1.5, p=0.2). AYA with NHL treated at community sites had worse outcome as compared to children (15-21y vs 1-14y: HR=2.4, p=0.04; 22-39y vs 1-14y: HR=3.9, p<0.01). The difference in outcome was diminished by care at NCICCC/COG (young AYA vs children with NHL: HR=2.0, p=0.06; older AYA vs children: HR=1.6, p=0.2). Compared to children and young AYA (1-21y) with HL, older AYA cared for at community sites had poor outcome (HR=2.2, p<0.01). The difference between older AYA and younger patients (1-21y) was mitigated by care at NCICCC (HR=1.2, p=0.6).
While 69% of children were treated at one of NCICCC/COG sites in LA County, only 38% of young AYA were seen at NCICCC/COG and merely 10% of older AYA were seen at NCICCCs. Compared with children (0-14y), young AYA (15-21y) were less likely to receive care at NCICCC/COG (ALL: OR=0.5; AML: OR=0.2; NHL: OR=0.3; HL: OR=0.2; all p<0.01), irrespective of SES, distance to care, insurance status. In analyses restricted to older AYA (22-39y), public or no insurance (ALL: OR=0.1; AML: OR=0.2; NHL: OR=0.3, all p<0.01), African-American or Hispanic background (HL: OR=0.3, p<0.01), low SES (NHL: OR=0.5, p<0.01) and distance from the nearest NCICCC (NHL: OR=0.5; HL: OR=0.5, all p<0.01) reduced likelihood of receiving care at NCICCC.
Conclusions:
Population-based data reveal that receipt of care at NCICCC/COG greatly diminishes the inferior outcome in AYA with hematologic malignancies. The role that cancer biology, therapeutic strategy and treating physician specialty (pediatric vs adult) each play in this dynamic is currently under investigation. Irrespective of all sociodemographic variables, young AYA are less likely to use NCICCC/COG than children. Among older AYA, patients without private insurance, from low SES, African-American/ Hispanic backgrounds or living >9 miles from the nearest NCICCC are less likely to receive treatment at NCICCC. Barriers to care at COG/NCICCC are currently being explored.
Stock:Jazz Pharmaceuticals: Consultancy; Amgen: Consultancy; Seattle Genetics: Consultancy; Sigma Tau: Consultancy; Sigma Tau: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.