Abstract

Introduction
Incidental pulmonary embolism (IPE) is defined as a pulmonary embolism diagnosed on a CT-scan performed for reasons other than a clinical suspicion of PE. Generally identified on staging scans, IPE has been estimated to occur in 3.1% of all cancer patients and is a growing challenge for clinicians and patients. Nevertheless, knowledge about the treatment and prognosis of cancer-associated IPE is scarce. In order to determine the outcome more accurately, and to identify clinical characteristics related to the prognosis, we pooled individual patient data from eleven observational studies and ongoing registries.
Methods
A systematic literature search aiming to identify studies reporting on patients diagnosed with cancer-associated IPE was performed. Authors of selected studies were invited to participate. Incidence rates of objectively diagnosed symptomatic recurrent venous thromboembolism (VTE), major bleeding and mortality during 6-month follow-up were pooled. Individual patient data was collected to perform subgroup analyses, for which all patients were considered as one cohort. Hazard ratios (HR) were adjusted for age, sex and cancer stage.
Results
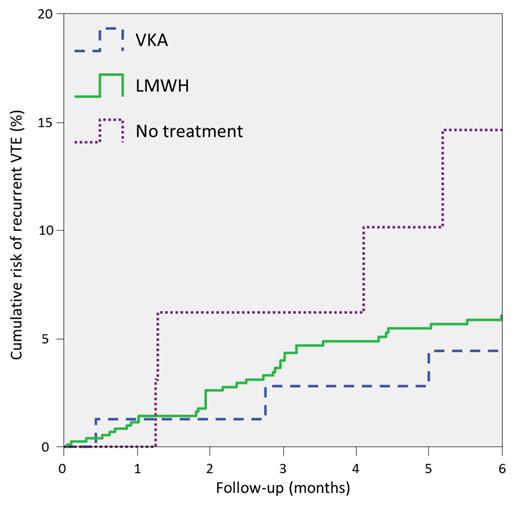
Individual patient data of 926 cancer patients with IPE from 11 observational studies and ongoing registries were included (Table 1). The overall pooled 6-month risk of symptomatic recurrent VTE was 5.8% (95%CI 3.7-8.3), of major bleeding 4.7% (95%CI 3.0-6.8) and of mortality 37% (95%CI 28-47). The VTE recurrence risk was comparable in patients treated with VKA and LMWH with incidence rates of 6.4% (95%CI 2.2-12) and 6.2% (95%CI 3.5-9.6), HR 0.89 (95%CI 0.27-2.9). In contrast, this incidence rate was 12% (95%CI 4.7-23) in patients who were left untreated, HR 2.9 (95%CI 0.65-13; Figure 1). The risk of major bleeding was significantly higher in patients treated with VKA compared to those treated with LMWH, 13% (95%CI 6.4-20) versus 3.9% (95%CI 2.3-5.9), HR of 3.2 (95%CI 1.4-7.4) (Figure 2). The 6-month mortality was 37% (95%CI 29-44) in patients treated with LMWH, 28% (95%CI 18-40) in those treated with VKA and 47% (95%CI 28-66) amongst untreated patients. The all-cause mortality at 6 months was significantly higher for patients with a central thrombus (either central or lobar) compared to those with a more peripheral IPE (either segmental or subsegmental); 42% (95%CI 33-52) versus 30% (95%CI 25-36, HR 1.8 (95%CI 1.4-2.3).
Conclusions
The most important finding of this study is the 12% 6-month risk of symptomatic recurrent VTE in patients with cancer-associated IPE who did not receive anticoagulant treatment, which is more than double the risk of patients who were anticoagulated. These numbers recall the effect size of anticoagulants used in symptomatic PE and support the judicious initiation of anticoagulant treatment in cancer-associated IPE. The association between more centrally-located thrombi and mortality following IPE is a new finding that parallels outcomes for symptomatic PE, and one which may further support similar management. Regarding the choice of anticoagulant, VKA were associated with a significantly higher risk of major bleeding than LMWH, with a comparable risk of recurrent VTE. The findings of this observational study should be preferably confirmed in a randomized trial.
The 6-month risk of major bleeding related to anticoagulant treatment.
Baseline characteristics
| Treatment | All patients n=926 (100%) | LMWH n=732 (79%) | VKA n=100 (11%) | No treatment n=53 (6%) | Other treatment n=41 (4%) | |
| Mean age (SD) | 65 (12) | 64 (12) | 68 (12) | 65 (14) | 68 (13) | |
| Male sex, n (%) | 491 (53) | 378 (52) | 60 (60) | 31 (58) | 22 (54) | |
| Cancer stage, n (%) | ||||||
| Metastatic | 501 (54) | 400 (55) | 56 (56) | 33 (62) | 12 (29) | |
| Non-metastatic | 192 (21) | 143 (20) | 34 (34) | 12 (23) | 3 (7.3) | |
| Unspecified | 233 (25) | 189 (26) | 10 (10) | 8 (15) | 26 (63) | |
| Cancer type, n (%) | ||||||
| Lung | 176 (19) | 135 (18) | 16 (16) | 18 (34) | 7 (17) | |
| Colorectal | 185 (20) | 150 (20) | 20 (20) | 9 (17) | 6 (15) | |
| Other gastrointestinal | 187 (20) | 147 (20) | 15 (15) | 13 (25) | 12 (29) | |
| Breast | 65 (7.0) | 52 (7.1) | 10 (10) | 1 (1.9) | 2 (4.9) | |
| Gynaecological | 64 (6.9) | 56 (7.7) | 5 (5.0) | 0 (0) | 3 (7.3) | |
| Other | 206 (22) | 155 (21) | 31 (31) | 10 (19) | 10 (24) | |
| Haematological | 43 (4.6) | 37 (5.1) | 3 (3.0) | 2 (3.8) | 1 (2.4) | |
| Largest artery involved, n (%) | ||||||
| Central | 292 (32) | 230 (31) | 30 (30) | 11 (21) | 21 (51) | |
| Peripheral | 495 (53) | 395 (54) | 62 (62) | 29 (55) | 9 (22) | |
| Unspecified | 139 (15) | 107 (15) | 8 (8.0) | 13 (25) | 11 (27) | |
| Treatment | All patients n=926 (100%) | LMWH n=732 (79%) | VKA n=100 (11%) | No treatment n=53 (6%) | Other treatment n=41 (4%) | |
| Mean age (SD) | 65 (12) | 64 (12) | 68 (12) | 65 (14) | 68 (13) | |
| Male sex, n (%) | 491 (53) | 378 (52) | 60 (60) | 31 (58) | 22 (54) | |
| Cancer stage, n (%) | ||||||
| Metastatic | 501 (54) | 400 (55) | 56 (56) | 33 (62) | 12 (29) | |
| Non-metastatic | 192 (21) | 143 (20) | 34 (34) | 12 (23) | 3 (7.3) | |
| Unspecified | 233 (25) | 189 (26) | 10 (10) | 8 (15) | 26 (63) | |
| Cancer type, n (%) | ||||||
| Lung | 176 (19) | 135 (18) | 16 (16) | 18 (34) | 7 (17) | |
| Colorectal | 185 (20) | 150 (20) | 20 (20) | 9 (17) | 6 (15) | |
| Other gastrointestinal | 187 (20) | 147 (20) | 15 (15) | 13 (25) | 12 (29) | |
| Breast | 65 (7.0) | 52 (7.1) | 10 (10) | 1 (1.9) | 2 (4.9) | |
| Gynaecological | 64 (6.9) | 56 (7.7) | 5 (5.0) | 0 (0) | 3 (7.3) | |
| Other | 206 (22) | 155 (21) | 31 (31) | 10 (19) | 10 (24) | |
| Haematological | 43 (4.6) | 37 (5.1) | 3 (3.0) | 2 (3.8) | 1 (2.4) | |
| Largest artery involved, n (%) | ||||||
| Central | 292 (32) | 230 (31) | 30 (30) | 11 (21) | 21 (51) | |
| Peripheral | 495 (53) | 395 (54) | 62 (62) | 29 (55) | 9 (22) | |
| Unspecified | 139 (15) | 107 (15) | 8 (8.0) | 13 (25) | 11 (27) | |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract