Abstract

Minimal residual disease (MRD) has been demonstrated to be of high and independent prognostic value prior to hematopoietic stem cell transplantation (HSCT) in childhood acute lymphoblastic leukemia (ALL) by several studies. Within the ALL-REZ BFM 2002 trial, MRD of 10-3 has been identified as the best prognostic cut-off before HSCT in children with relapsed ALL. In this study we have investigated, whether interventional treatment intensification in patients with persisting MRD at a level of =/>10-3 is capable of reducing MRD prior to HSCT and improving survival.
In the trial ALL-REZ BFM 2002 (recruitment of patients between 01'2002 and 09'2012) online MRD-monitoring has been performed in patients with ALL relapse and indication for allogeneic HSCT since 2010. MRD results obtained during the consolidation treatment phase and before HSCT have been disclosed to the treating centers. Treatment courses consisting of Clofarabine/Cyclophosphamide/Etoposide, Daunoxome or Idarubicine/Fludarabine/Cytarabine, or in case of T-ALL Nelarabine alone or with Cyclophosphamide/Etoposide were offered as interventional elements and administered to patients at the discretion of the treating physician aiming at reducing MRD and improving survival. A total of 30 patients with first ALL relapse and persisting MRD at a level of =/>10-3 at the end of consolidation treatment received an interventional intensification before HSCT (Intervention Group, IVG). Sixty patients with first relapse and persisting MRD at a level of 10-3 at the end of consolidation treatment did not receive an interventional intensification before proceeding to HSCT (non-IVG).
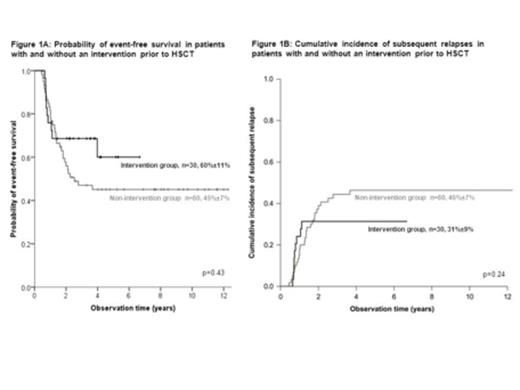
MRD reduction of at least one log step was achieved in 78% and of two log steps in 59% of patients after interventional intensification. Relevant clinical characteristics as time to relapse, site of relapse, immunophenotype, consolidation treatment arm and type of HSCT were equally distributed between the IVG and the non-IVG. However, the proportion of patients with an MRD levels <10-3 and <10-4 was significantly higher in the IVG with 83% and 71% than in the non-IVG with 48% and 18%, respectively (p=0.005 and p<0.001). There were no significant differences in the probability of event-free survival at 5 years (60% +/-11% vs 45% +/-7%, Figure 1A), and the cumulative incidence of subsequent relapse (31% +/-9% vs 46% +/-7%, Figure 1B) or of therapy related death (0% +/-0% vs 8% +/-4%) between the IVG and non-IVG. Including only patients with MRD reduction of at least two log steps after interventional intensification (n=16), the probability was 59% +/-16% in the IVG compared to 45% +/-7% in the non-IVG (p=0.24).
In conclusion, persisting MRD during consolidation treatment can be efficiently reduced by interventional intensified chemotherapy. However, this does not translate into a significant improvement of survival. MRD persistence after intensive conventional chemotherapy seems to identify particularly aggressive leukemias which are not successfully treated by further reduction of the MRD load. Therefore, targeted therapies need to be investigated and prospective controlled studies should be given preference to individualized interventions.
von Stackelberg:Amgen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract