Abstract

In younger patients with acute myeloid leukemia (AML), standard intensive induction chemotherapy combines anthracyclins and cytarabine (Ara-C). While dosage is usually determined according to body-surface area (BSA), various chemotherapy adjustments are empirically performed in patients with high BSA from full dose administration to capping doses. The aim of the present study is to determine the outcome of younger AML patients with high BSA at diagnosis.
Between November 2001 and April 2005, the prospective GOELAMS 2001 trial enrolled patients between 18 and 60 affected with non promyelocytic AML.1,2 Briefly, patients randomly received either daunorubicin or idarubicin in association with standard dose Ara-C during induction therapy. Height, weight and induction chemotherapy doses were registered at diagnosis. BSA was evaluated using the formula of Dubois and Dubois. BSA was categorized in low (BSA ≤1.5m2), intermediate (1.5<BSA<2), high (2<BSA<2.15) or very high BSA (BSA ≥2.15). In the course of consolidation therapy, patients with a matched related donor received an allogeneic stem cell transplantation. Patients without a matched related donor received either a single or tandem autologous bone marrow transplantation. Patients who did not achieve sufficient stem cell mobilization received chemotherapy-only consolidation.
823 patients were eligible to induction therapy. 43 (5%), 638 (77%), 91 (11%) and 51 (6%) patients displayed low, intermediate, high or very high BSA at diagnosis, respectively. Median age, performance status, karyotype group were similar in all BSA groups. On the contrary, male gender was enriched in high and very high BSA groups (86% and 88%, respectively). During induction therapy, 20 patients (39%) with very high BSA were administered reduced dose (decrease of > 10% in anthracyclin or Ara-C dosing compared to full dose) versus 8%, 4% and 7% in low, intermediate or high BSA subgroups (p <10-5). Type of consolidation therapy - chemotherapy, autologous or allogeneic stem cell transplantation - was not significantly different in BSA groups.
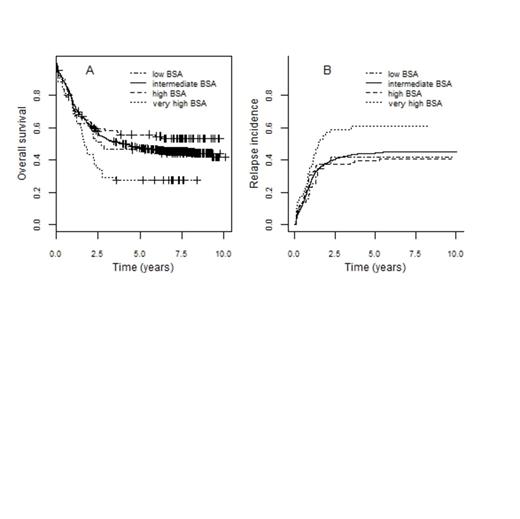
Compared to patients with intermediate BSA, patients with a low or high BSA displayed a similar OS and EFS. On the contrary, patients with a very high BSA displayed a decreased 5-year OS (27% (95% CI, 18-43) vs 47% (95% CI, 44-51), p= 0.006, figure 1A) and LFS (22% (95% CI, 13-36) vs 41% (95% CI, 37-45), p=0.004). Non-relapse mortality was similar in the very high or intermediate BSA groups, suggesting that intensive therapy was similarly tolerated in intermediate or very high BSA patients. Meanwhile, relapse incidence was increased in patients with a very high BSA compared to intermediate BSA patients (61% (95% CI, 46-73) vs 44% (95% CI, 40-48), p = 0.02, figure 1B).
Conclusion: patients with a very high BSA display an adverse outcome, due to an increased relapse incidence. Meanwhile, non-relapse mortality is not significantly increased in very high BSA patients. These data suggest that patients with very high BSA should receive full dose induction chemotherapy.
Bibliography;
1. Recher C , Bene MC, Lioure B et al. Leukemia, Long-term results of a randomized phase 3 trial comparing idarubicin and daunorubicin in younger patients with acute myeloid leukaemia. Leukemia 2014; 28:440-3.
2. Lioure B, Bene MC, Pigneux A et al. Early matched sibling hematopoietic cell transplantation for adult AML in first remission using an age-adapted strategy: long-term results of a prospective GOELAMS study. Blood 2012; 119: 2943–2948.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract