Abstract
Toxicity and drug resistance has impeded clinical improvements in acute myeloid leukaemia (AML). We hypothesized that directly targeting pro-survival proteins with BH3-mimetics may have therapeutic rationale in AML and potentially sensitize chemoresistant cases to chemotherapy. This work will therefore assess which Bcl-2 family members mediate pro-survival activity in AML and the potential benefit of combining BH3-mimetics with standard AML drugs.
Immunoblotting of fresh primary AML samples revealed strong Bcl-2 expression in 12/13 (92%) cases, Bcl-xL expression in 3/13 (23%) cases and Mcl-1 expression in 8/13 cases (62%). Sensitivity to ABT-199 (targets Bcl-2) or ABT-737 (targets Bcl-2, -xL, -w) was assessed by incubation of freshly harvested AML samples in RPMI + 20% FBS for 48 hrs and viable cells enumerated by exclusion of Sytox Blue using flow cytometry. There were 2 discrete populations identified; one that was sensitive to ABT-199 with an LC50 (concentration of drug to kill 50% of AML blasts) < 10nM (5/13 cases; 39%) and a more resistant population (LC50 > 10μM in 6/13 cases, 46%). A strong correlation in the sensitivity of AML cells to ABT-199 and ABT-737 was observed (r=0.9628, p < 0.0001), suggesting Bcl-xL was not a dominant survival factor in AML.
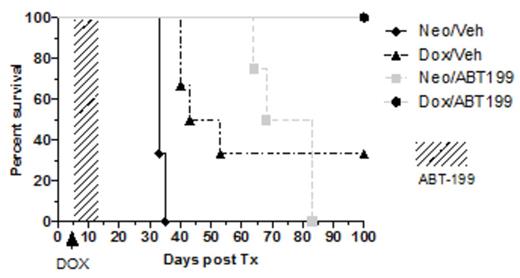
To identify relevant Bcl-2 pro-survival targets for elimination of AML in vivo, MV4;11 cells were engineered to express under doxycycline control 1) BimSwt targeting all pro-survival proteins, 2) BimS2A targeting Mcl-1 only, 3) BimSBad targeting Bcl-2, -x and –w; or 4) an inert BimS4E, which served as a negative control. 1x 105 MV4;11 cells per mouse were xenografted into cohorts of 6 NSG mice and doxycycline-rich water introduced on day 5 after transplantation. Mice transplanted with MV4;11 cells expressing the inert BimS4E succumbed to leukemia by ~ day 40. Expression of BimSBad or BimS2A delayed, but did not prevent leukemia-related death, whereas mice engrafted with MV4;11 cells enforced to express BimSwt were alive and leukemia-free after 100 days (Figure 1A). Similar outcomes were demonstrated using an OCI-AML xenograft model (not shown). As on-target toxicity to platelets is an undesirable consequence of targeting Bcl-xL (Mason, Cell 2006), the effectiveness of targeting only Bcl-2 and Mcl-1 in vivo was next investigated. Mice engrafted with MV4;11 cells expressing BimS2A (to target Mcl-1) were fed doxycycline water from day 5 onwards. In addition, the selective Bcl-2 inhibitor ABT-199 75mg/kg was administered daily by oral gavage between days 5-12 post engraftment. Strikingly, this combination strategy led to eradication of AML by day 100 in all mice, in contrast to delayed, but inevitable leukemic death in most mice receiving treatment directed at either Bcl-2 (ABT-199) or Mcl-1 (Bims2A) alone (Figure 1B). These results suggest that AML eradication in vivo is best achieved through combined targeting of Bcl-2 and Mcl-1. In the absence of direct inhibitors of Mcl-1, standard AML drugs were examined for their capacity to suppress Mcl-1. In the MV4;11 cell line, anthracyclines such as idarubicin rapidly (< 3 hrs) suppressed Mcl-1 at concentrations between 300nM and 1μM. In contrast, 100μM cytarabine did not suppress Mcl-1 after exposure for 6 hrs. Further studies in primary AML cells demonstrated synergy between ABT-199 and idarubicin in ABT-199 resistant AML cells.
We conclude that 1) a subset of primary AML cells is highly sensitive to Bcl-2 inhibition, 2) that eradication of AML in vivo is best through combined Bcl-2/Mcl-1 targeting and 3) that anthracyclines are effective at suppressing Mcl-1 and could be combined with ABT-199 to treat patients with AML resistant to Bcl-2 targeted therapy.
A
A) Cohorts of 6 NSG mice were xenografted with MV4;11 cells expressing BimS ligand variants under doxycycline control. Doxycycline water was fed to mice from day 5+ and survival assessed. B. Cohorts of 6 NSG mice were xenografted with MV4;11 cells expressing BimS2A under doxycycline control. Mice were allocated to treatment with either vehicle or ABT-199 on days 5-12 +/- doxycycline water from day 5+ and survival assessed. All mice in the arm combining Doxycycline (to suppress Mcl-1) and ABT-199 (to target Bcl-2) were alive and leukemia-free on day 100.
A) Cohorts of 6 NSG mice were xenografted with MV4;11 cells expressing BimS ligand variants under doxycycline control. Doxycycline water was fed to mice from day 5+ and survival assessed. B. Cohorts of 6 NSG mice were xenografted with MV4;11 cells expressing BimS2A under doxycycline control. Mice were allocated to treatment with either vehicle or ABT-199 on days 5-12 +/- doxycycline water from day 5+ and survival assessed. All mice in the arm combining Doxycycline (to suppress Mcl-1) and ABT-199 (to target Bcl-2) were alive and leukemia-free on day 100.
B
Huang:AbbVie: Consultancy, Honoraria. Wei:Abbvie: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.