Abstract
SUMMARY
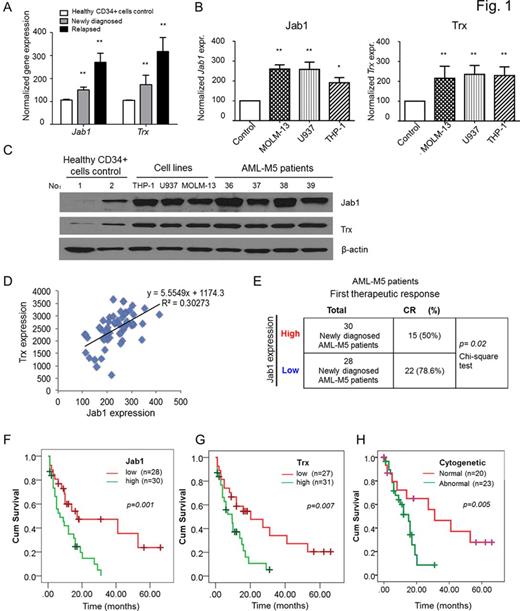
Increased production of reactive oxygen species (ROS) or an inefficient antioxidant system leads to oxidative stress, which influences hematopoietic cell function in acute myeloid leukemia (AML); however, the mechanisms of this stress remain poorly understood. Investigations were carried out on matched samples from the same 58 patients with AML-M5 (33 males and 25 females) who experienced a relapse after treatment. They had a median age of 43.90 ± 17.39 years (range, 14-77 years) at diagnosis and 44.86 ± 16.28 years at relapse. The mean white blood cell (WBC) counts were 16.58 x 109/L at diagnosis and 24.41 x 109/L at relapse (P < 0.05). Here, our studies showed that abnormally high ROS levels and low antioxidant enzyme capacity were characteristic of AML-M5 at both diagnosis and relapse. It is worth mentioning Jab1 and Trx protein levels were higher in all leukemia cell lines tested (THP-1, U937, and MOLM-13 cells), as well as in leukemic cells derived from AML-M5 patients, than in CD34+ cells from healthy donors (Figure 1A-D). A chi-square test revealed that patients with high Jab1 levels were less sensitive to Ara-c-based chemotherapy (Figure 1E). Consistently, high gene expression levels of thioredoxin (Trx) and Jab1 were associated with poor survival rates in AML-M5 patients(Figure 1F-H). Moreover, stimulating AML-M5 cells with a low concentration of hydrogen peroxide increased Jab1 and Trx expression. Additionally, depletion of Jab1 inhibited cellular proliferation and invasion, which was accompanied by a decrease in Trx expression.
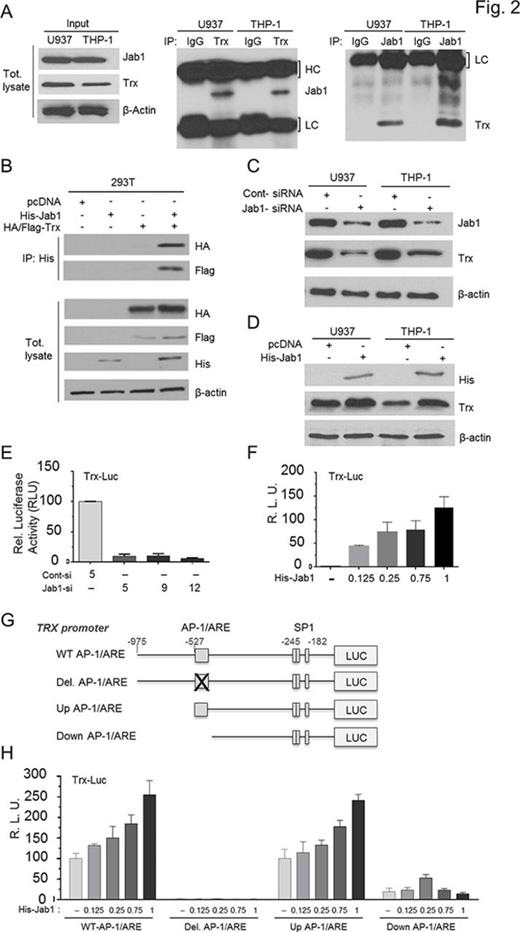
Mechanistically, we demonstrate that Jab1 controls a major antioxidative cellular molecule Trx by interacting with and enhancing its transcriptional levels through AP-1 binding sites. To assess whether Jab1 and Trx interact we performed co-immunoprecipitation assays and demonstrated that Jab1 and Trx proteins interacted specifically with each other using endogenous proteins or ectopically expressed tagged-proteins, in U937 and THP-1 cells (Figure 2A and B). Furthermore, our results demonstrate that Jab1 knockdown remarkably reduced Trx levels (Figure 2C). Inversely, Jab1 overexpression induced higher endogenous Trx levels (Figure 2D). However, neither Trx silencing nor Trx overexpression affected Jab1 levels. Thus, our findings indicate that Jab1 is an upstream regulator and positively controls Trx expression in AML-M5 cells. To further delineate whether Jab1 regulates transcriptionally Trx, we performed a luciferase reporter assays with the human Trx promoter. Our data demonstrated that transactivation of Trx expression is driven by Jab1 through the AP-1 binding site (Figure 2E-H). In conclusion, these results elucidate a novel Jab1 and Trx axis, which is a critical cellular process in the pathobiology of AML-M5 and could promotes AML-M5 relapse.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.