Abstract
Background: The risk of cancer- and catheter-associated thrombosis in patients with diffuse large B-cell lymphoma (DLBCL) receiving R-CHOP chemotherapy (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) has not been well characterized yet.
Methods & Materials: Medical records of patients who diagnosed with DLBCL and treated with R-CHOP chemotherapy for the first-line between January 2006 and December 2014 in Severance hospital were reviewed retrospectively. The patients who had imaging study for response evaluation after completion of at least 3 cycles of R-CHOP or the patients who were confirmed to have thrombosis before 3cycles of chemotherapy were included. Catheter-associated thrombosis was defined as mural thrombosis extending from the catheter into the lumen of a vessel and leading to partial or total catheter occlusion. Extended cervical structure was defined as the structure from the area of low cervical nodes (station 1) according to International Association for the Study of Lung Cancer (IASLC) lymph node map to the area of nasopharynx and tonsil. Thrombotic events which occurred within 1 year after diagnosis of DLBCL were analyzed. The patients without thrombotic events were censored at 1 year after diagnosis of DLBCL or at the date of last follow up. The risk of thrombotic events was compared using Kaplan-Meier method or Cox regression analysis. A two-tailed P < 0.05 was considered significant.
Result: A total of 528 patients (304 male and 224 female) were studied. Median age was 57 years (range 17-88). 518 patients (98.1%) received R-CHOP chemotherapy via implanted port. Overall 55 thrombotic events (10.4%) were occurred within 1 year after diagnosis of DLBCL. Cancer-associated and catheter-associated thrombosis were occurred in 38 (7.2%) and 18 (3.4%) patients, respectively. Sites of cancer-associated thrombosis were as followed: pulmonary thromboembolism (PTE, 42.1%), deep vein thrombosis (DVT) without PTE (36.8%), DVT with PTE (10.5%) and stroke (10.5%).
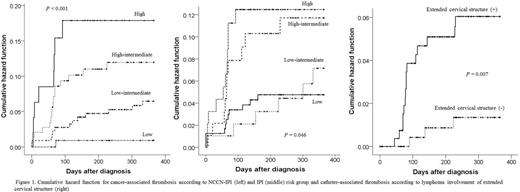
In univariate analysis for cancer-associated thrombosis, age >60 years (P = 0.008), Ann-arbor stage >2 (P = 0.003), performance state >1 (P = 0.013), extranodal involvement >1 (P = 0.001), normalized LDH >1.5 (P = 0.001), WBC >9,000/mL (P = 0.004), hemoglobin <10 g/dL (P = 0.033), body mass index (BMI) >25.0 (P = 0.024) and patient group of higher risk according to International Prognostic Index (IPI, P = 0.046, figure 1) and NCCN-IPI (P < 0.001, figure 1) were associated with increased risk of thrombosis. Gender, BMI >35, WBC >11,000/mL, platelet >350K/mL, use of erythropoietin, and B-symptom did not show significance. In multivariate analysis, NCCN-IPI (P = 0.017), WBC >9,000/mL (odds 2.100; 95% CI 1.023-4.307; P = 0.043), BMI >25.0 (odds 2.177; 95% CI 1.139-4.160; P = 0.019) except hemoglobin <10 g/dL (P = 0.369) showed significance. However, when IPI was included in multivariate analysis instead of NCCN-IPI, IPI did not show significant association (P = 0.178).
In univariate analysis for catheter-associated thrombosis, age <61 years (P = 0.009), B-symptom (P = 0.029), and lymphoma involving extended cervical structure (P = 0.007, figure 1) were associated with increased risk of thrombosis. Other factors that were associated with cancer-associated thrombosis were not significantly associated. In multivariate analysis, lymphoma involvement of extended cervical structure (odds 4.689; 95% CI 1.357-16.207; P = 0.015), age <61 (odds 5.996, 95% CI 1.376-26.121; P = 0.017), and B-symptom (odds 2.658; 95% CI 1.048-6.743; P = 0.40) showed significance.
Conclusion: Our data suggest that the patients with higher NCCN-IPI risk group, WBC >9,000/mL, and BMI >25.0 may be associated with increased risk of cancer-associated thrombosis. Unlike NCCN-IPI, IPI lost its significance for cancer-associated thrombosis after multivariate analysis. The risk of catheter-associated thrombosis was increased in patients with B-symptom and having lymphoma involving extended cervical structure but not in older patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.