Abstract
Introduction
Allogeneic BMT is often the only curative option for poor-risk AML. Not only does mismatched BMT circumvent the limited availability of HLA matched donors, but it also allows a wider choice of potential donors. We report an analysis of mini-haplo BMT in 93 patients with high-risk AML. In light of emerging data regarding the influence of donor age on outcome of BMT, we specifically studied the impact of donor age on outcome.
Methods We conducted a retrospective review of all adult patients at Johns Hopkins, who received a mini-haplo BMT for AML between January of 2003 and February of 2013. Patients received Cy (14.5 mg/kg/day IV D -6,-5), fludarabine (30mg/mg2/day IV D -6 to -2), and 200 cGy total body irradiation on day -1. GVHD prophylaxis was PTCy (50 mg/kg D 3, 4), mycophenolate mofetil, and tacrolimus. Progression-free (PFS) and overall survival (OS) were evaluated based on Kaplan-Meier method. The cumulative incidence of GVHD and non-relapse mortality (NRM) were assessed via Gray's approach..
Results
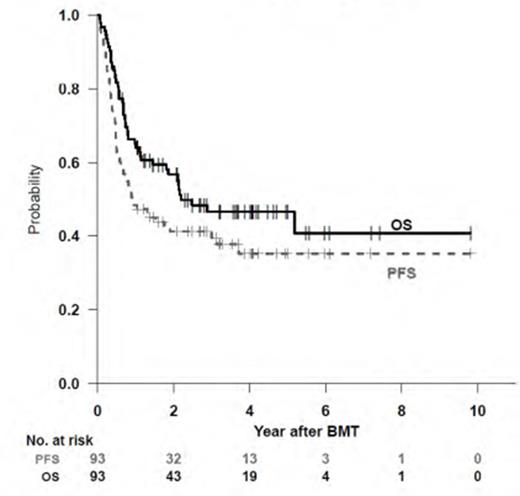
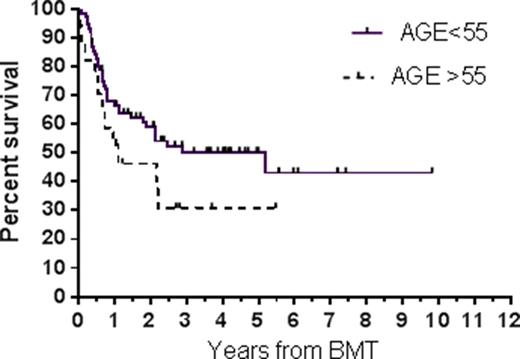
The median age of the 93 AML patients was 54 (range 24-73). For the 47 patients transplanted in CR1, the median time to BMT from CR1 was 84 (range 11-347) days. Median follow-up was 44 (range 5-117) months. Successful engraftment with sustained donor chimerism was achieved in 80 of 89 evaluable patients by day 60; two additional patients experienced secondary graft failure. These 11patients who developed graft failure had donors who were older, with a median age of 49 (range 35-63) versus 38 (range 14-68) years (p=0.03), and they received allografts with significantly fewer CD34+ cells, with a median of 2.5x106/kg compared to 4.5x106 cells/kg (p=0.01). The 13 allografts with ≤ 2.5x106 CD34+ cells/kg were associated with 6 of the primary graft failures compared to only 5 graft failures in the 80 patients receiving > 2.5x106 CD34+ cells/kg (p=0.0004). Moreover, the donors of the 13 allografts with ≤ 2.5x106 CD34+ cells/kg had a median age of 52 compared to age 39 for donors of the 80 grafts with > 2.5x106 CD34+ cells/kg (p=0.04). The overall cumulative incidence (CI) of grade II-IV and III-IV aGVHD and cGVHD was 24% (95% CI 15-33%), 8% (2-13%), and 17% (9-25%), respectively. The CI of NRM was 11% (4-17%). The overall CI of relapse was 54% (95%CI 43-65%). The 4-year actuarial OS and PFS were 47% (95% CI 37-59%) and 35% (95%CI 26-48%) (Fig 1). Patient age did not have a significant impact on survival. However, there was a trend toward better survival with younger donors. For patients with donors ≤ 55 years, the median OS was 63 (range 1-118) months compared to 13 (range 1-65) months (p=0.14) (Fig 2).
Discussion
Mini-haplo BMT offers a potentially curative option for poor-risk AML patients lacking matched donors. GVHD and NRM rates were low. The time to BMT in our patients was similar to those reported for matched sibling donors (Walter, et al, Blood. 2013; 122: 1813-1821) and shorter than those for MUD transplants, (Rollig, et al, JCO. 2015; 33: 403-410), an important consideration because over one-third of pts with high-risk AML relapse within 4 months of initial therapy. Graft failure, a concern with mismatched BMT, appears to be in part related to donor age, with older donors providing inferior quality allografts. Survival was also inferior with the use of older donors. Our data strongly suggest that no AML patient in need of BMT should be denied the procedure for lack of a suitable donor. Moreover, the use of mismatched donors allows donor selection based on donor characteristics, such as age, that have the potential to improve outcomes.
Overall and progression-free survival of the entire cohort
Overall and progression-free survival of the entire cohort
Overall survival by donor age
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.