Abstract

Background: DLBCL relapsing after an auto-HCT has a poor prognosis. Unfortunately this is a common clinical dilemma, since ~50% of auto-HCTs for DLBCL ultimately fail. Allo-HCT is often considered following failure of an auto-HCT; however, limited information is available regarding prognostic factors identifying DLBCL patients likely to benefit from a subsequent allo-HCT.
Methods: Adult (≥18 years) DLBCL patients undergoing an alloHCT between 2000-2012, after experiencing disease progression/relapse (P/R) following a prior autoHCT and reported to the CIBMTR were included. Patients undergoing tandem auto-allo HCT and those receiving allo-HCT for indications other than relapsed DLBCL were excluded. Primary outcomes were non-relapse mortality (NRM), P/R, PFS, and overall survival (OS). Cox regression method was used to develop a prognostic model of PFS and OS.
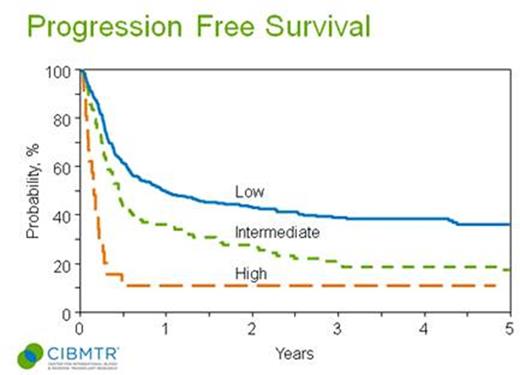
Results: Characteristics of 503 patients included in this analysis are shown in Table 1. The 3-yr univariate probabilities of NRM, P/R, PFS and OS were 30%, 38%, 31% and 37% respectively. Factors associated with higher NRM on multivariate analysis (MVA) included chemoresistance disease prior to allo-HCT (RR=1.86; p=0.003), myeloablative conditioning (MAC) (RR=1.99; p=0.0006; within 1st 10months following alloHCT) and unrelated donors (URD) grafts (RR=1.44; p=0.03). Factors associated with P/R on MVA included chemoresistance (RR= 2.25, p<0.0001), Karnofsky performance status (KPS) <80 (RR 1.81, p=0.006), and interval between auto-HCT and allo-HCT of <1 yr (RR=2.28, p<0.0001). Factors associated with inferior PFS on MVA included KPS <80 (RR=1.79, p=0.0005), chemoresistance (RR=2.04, p<0.0001), auto-HCT to allo-HCT interval <1 yr (RR=1.32, p=0.01), and MAC (RR 1.29, p=0.03). Factors associated with worse OS on MVA included KPS <80 (RR1.86, p=0.0003), chemoresistance (RR=1.94, p<0.0001), MAC (RR=1.39, p=0.008). Three adverse prognostic factors were used to construct a prognostic model for PFS, including; (i) KPS <80 (2 points) (ii) Interval between auto-HCT & allo-HCT of <1yr (1 point) and (iii) chemoresistant disease at allo-HCT (2 points). This CIBMTR prognostic model classified patients into three prognostic groups: low risk (0-1 points), intermediate risk (2-3 points), or high risk (4-5 points), predicting 3-yr PFS probabilities of 38% (95% CI=32-44), 19% (95% CI=11-27) and 10% (95% CI=0-22), respectively (Fig 1). The 3-yr OS probabilities in similar order were 43%, 25% and 14% respectively.
Conclusion: The CIBMTR prognostic model identifies a subgroup of DLBCL patients relapsing from an auto-HCT who can experience long-term PFS following an allo-HCT. Reduced-intensity conditioning is preferred in this setting.
| . | N=503 (%) . |
|---|---|
| Median age at alloHCT, years | 52 (range 19-72) |
| Male gender | 305 (61) |
| KPS ≥80 | 393 (78) |
| Stage III-IV at diagnosis | 54% |
| Rituximab prior to HCT | 72% |
| Median lines of therapy | 4 (range 1-7) |
| High LDH at HCT | 34% |
| Time from auto-HCT to allo-HCT, months | 15 (range 1-198) |
| Disease status at transplant | |
| CR | 175 (35) |
| PR | 197 (39) |
| Chemorefractory | 106 (21) |
| Untreated | 12 (2) |
| Missing | 13 (3) |
| Type of donor | |
| Sibling | 253 (50) |
| URD | 250 (50) |
| Myeloablative conditioning | 127 (25) |
| PB graft | 456 (91) |
| TBI in conditioning | 133 (26) |
| Median follow up, months | 55 (range 1-149) |
| . | N=503 (%) . |
|---|---|
| Median age at alloHCT, years | 52 (range 19-72) |
| Male gender | 305 (61) |
| KPS ≥80 | 393 (78) |
| Stage III-IV at diagnosis | 54% |
| Rituximab prior to HCT | 72% |
| Median lines of therapy | 4 (range 1-7) |
| High LDH at HCT | 34% |
| Time from auto-HCT to allo-HCT, months | 15 (range 1-198) |
| Disease status at transplant | |
| CR | 175 (35) |
| PR | 197 (39) |
| Chemorefractory | 106 (21) |
| Untreated | 12 (2) |
| Missing | 13 (3) |
| Type of donor | |
| Sibling | 253 (50) |
| URD | 250 (50) |
| Myeloablative conditioning | 127 (25) |
| PB graft | 456 (91) |
| TBI in conditioning | 133 (26) |
| Median follow up, months | 55 (range 1-149) |
Smith:Celgene: Consultancy; Pharmacyclics: Consultancy. Sureda:Seattle Genetics Inc.: Research Funding; Takeda: Consultancy, Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract