Abstract
Background: Thrombocytopenia during heparin administration is common in hospitalized patients, leading to frequent testing for heparin-induced thrombocytopenia (HIT). The 4T score, which is based on degree and timing of thrombocytopenia, and whether there are other explanations for thrombocytopenia or the presence of thrombosis, is a commonly used tool to assess the clinical probability of HIT prior to performing laboratory testing. Published guidelines recommend further testing with an anti-PF4/heparin enzyme immunoassay (EIA) and confirmation with the serotonin-release assay (SRA) when the pretest probability of HIT is intermediate or high. The diagnosis of HIT confers high morbidity and mortality; therefore it is crucial to establish a definitive diagnosis in patients with suspected HIT. However, empiric treatment with alternative non-heparin anticoagulants increases the cost of hospitalization and may cause unnecessary risks in patients with a false positive EIA. The purpose of our study was to evaluate the utilization of EIA and SRA at a large tertiary care center and to assess the agreement between the 4T score, the EIA, and the SRA.
Methods: We retrospectively reviewed all EIAs performed in our special hematology laboratory and SRAs sent to a reference laboratory at our institution in patients with suspected HIT between July 2012 and June 2014. First we evaluated the 4T score in all patients in whom laboratory testing was requested and subsequently assessed the correlation between the 4T score and the EIA and SRA results. A 4T score of 6 to 8 was high and a 4T score of 4 to 5 was intermediate. A strong positive EIA was defined as an EIA with an optical density (OD) of ≥ 1.00 and a weak/indeterminate EIA had an OD of 0.40-0.99.
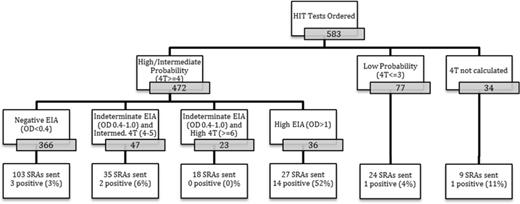
Results: A total of 583 unique PF4 EIAs were requested during the study period (Figure 1). Of these, 472 (81%) and 77 (13%) were performed in patients with intermediate/ high probability and with low-probability of HIT, respectively and in 34 patients (6%) the EIA was requested without documentation of the 4T score. Of the 472 patients with an intermediate or high 4T score, 36 (8%) had an EIA with an OD ≥ 1.0. Of these 36 patients, 27 (75%) had SRA performed and were positive in 14 patients (52%). Twenty-three (5%) of the 472 patients had a weakly positive EIA and in 18 (78%) of them the SRA was sent and were all negative. Five of the 472 patients (1%) had a positive SRA in the setting of an intermediate or high 4T score and a negative or indeterminate/weakly positive EIA. The SRA was sent in 24 patients with low probability 4T score (0-3) and in 9 patients with no documented 4T score. Two of these 33 (6%) patients had a positive SRA. Overall, the incidence of HIT based on a 4T score of 4 to 8, a positive EIA and positive SRA was found in 16 (3.4%) of the 472 patients; 2 of these 16 patients (12.5%) had a indeterminate/weakly positive EIA. Of the 216 SRAs sent, 21 were positive (9.7%). Patients with a lower pre-test probability based on a low or intermediate 4T score and negative/weakly positive EIA accounted for 33% of HIT cases observed. Patients with an intermediate/high 4T and strong or weakly positive EIA accounted for the remaining 67%.
Conclusions: The incidence of definitive HIT in our study was low. There was a poor correlation between the 4T score and SRA positivity and between the EIA and SRA results. The combination of an intermediate/high 4T score and a strong EIA confirmed the diagnosis of HIT in only half of the patients. These findings underscore the need for improved screening tools for HIT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.