Abstract

Introduction: Sickle Cell Disease (SCD) affects approximately 1 in 350 African American newborn infants each year in the United States and 70,000-100,000 people in the United States. Vaso-occlusive pain crisis is the most common complication that results in patients seeking emergency care for sickle cell disease. In the US in 2006, an estimated 232,381 emergency department (ED) visits were related to sickle cell disease, which resulted in approximately $356 million of ED health care costs and $2.6 billion of combined ED and inpatient costs. Initial pediatric data suggests that time to opiate initiation effectively decreased the total ED length of stay, and total intravenous opiates. While adult ED protocols have been implemented, results on time to first opiate as well as health care utilization has been variable.
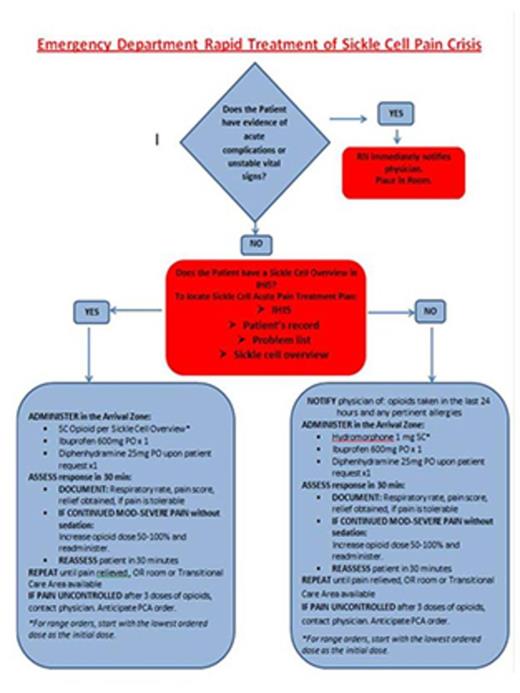
Methods: A multidisciplinary quality improvement group was formed to improve emergency room department care delivery for patients with sickle cell disease. The existing NIH 2014 sickle cell guideline and Tanabe protocol was modified to include individualized pain plans (Figure 1). The primary goal was defined as average time to first opiate of < 60 minutes. The secondary goal was to improve long term health care utilization as measures by length of ED stay and readmission rates for patients with sickle cell disease. The data was compared to a year prior to protocol implementation given the seasonal variations observed in patient admissions and encounter volumes. For reporting, those patients that require a toxicology screen prior to opiate administration were excluded from the data analysis.
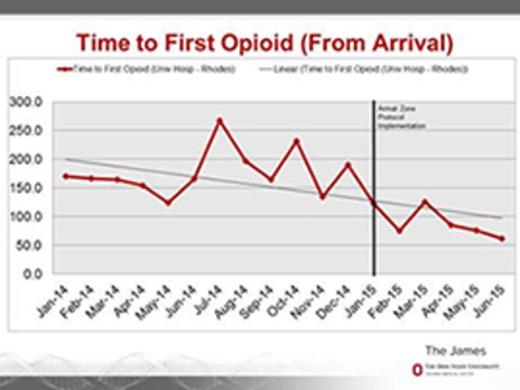
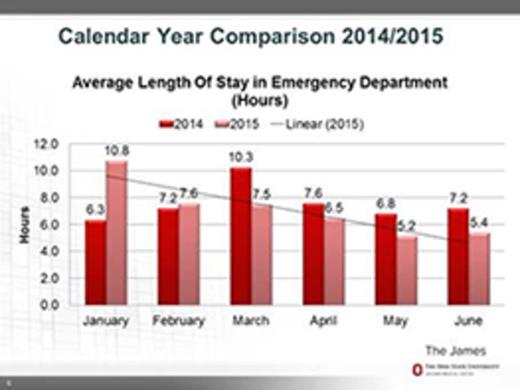
Results: There were a total of 352 encounters from 102 unique patients that occurred time of protocol initiation (January 2015-June 2015). The average time to first opiate in January 2014 was 170 min and June 2014 was 166min. After protocol implementation, the average time to first opiate in January 2015 was 123 min and June 2015 62 min (Figure 2). The readmission rate compared to May and June 2014 was decreased by 43% and 20% in May and June 2015, respectively. The average length of ED stay decreased from 9.4 hrs in June 2014 to 5.0 hrs in June 2015 (Figure 3).
Conclusion: With a collaborative multi-disciplinary approach, successful ED protocol implementation is feasible. The collaboration can lead to better patient care with improvement in time to analgesia. The model may also contribute to reduction in health care utilization.
Desai:Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract