Abstract

Background: The conventional treatment (CT) for beta- thalassemia major (TM) includes regular transfusion accompanied by iron-chelating therapy. However, this laborious treatment by given desferrioxamine (DFO) subcutaneously for 8 to12 hours per days, at least 5 days per week with/without deferiprone (DFP) has led to poor compliance, even though, the new medicine named deferasirox (DFX) has been introduced in China recent years. Nevertheless, the high cost makes it difficult to use widely for many families. Hematopoietic stem cell transplantation (HSCT) provides an alternative curative option for TM patients. To our knowledge, data from China has not been available in the literature on cost comparison between HSCT and CT.
Aims: The principal aim of our study is to compare the lifetime undiscounted mean cost (UMC) of hematopoietic stem cell transplantation (HSCT) with UMC of conventional therapy (CT) in beta-thalassemia major (TM) patients and to investigate the relationship of the clinical features to cost outcomes of HSCT.
Methods: We estimated UMC of 93 TM-HSCTs between 2011 and 2012 with a median age of 6 years (range, 3-16) and a median follow-up time of 3 years (range, 2.4 -3.8). The relationship between the UMC of HSCT and patient characteristics were analyzed. The UMC of 93 TM-HSCTs was compared with UMC of CT based on total 1526 TM patients. Age was used as matching variant, and the mean cost of each age was calculated, then cumulative cost was further adjusted for age in patients.
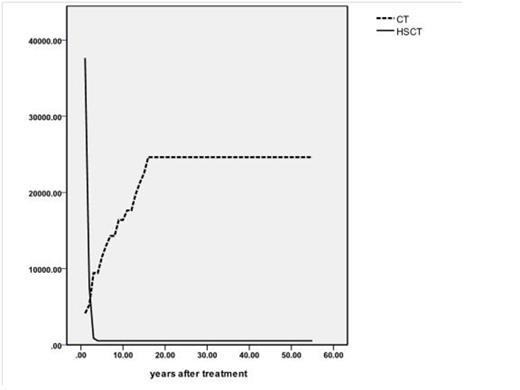
Results: UMC of TM-HSCT was CNY (Chinese Yuan) 235,254/USD 37,664 (95% confidence interval (CI) CNY208, 081-262,719/USD 33,293-42,035) with mean hospital stay of 60.5 days (95% CI 49-71). UMC of 20 years of follow-up and total undiscounted lifetime (55 years) for patients underwent HSCT were CNY 345,317/USD55, 251 and CNY 465,975/USD 74,602 respectively. However, the corresponding costs of patients undergoing CT were CNY 2,101,488/ USD336, 238 and CNY 7,489,519/ USD1, 198,323 respectively. Patient characteristics were helpless to predict the costs. HLA-mismatched transplants increased significantly UMC of HSCT than matched transplants (USD 35,818 vs. USD 52,771; p<0.001). The development of GVHD were associated with higher costs (USD 63,933 vs. USD 44,547; p = 0.001).
Conclusions: Cost comparison of HSCT and CT suggests that HSCT is an efficient and high cost-effective treatment for TM patients. Mismatched donor transplant increases the cost of HSCT.
Keywords: hematopoietic stem cell transplantation, iron overload, cost analysis
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract