Abstract
Introduction:
Sickle cell disease (SCD) is the leading cause of overt stroke in children, resulting in increased morbidity and mortality (Prengler et al. 2002). Neurologic injury in SCD is caused by a cascade of complex physiological processes that may manifest as abnormal cerebral blood flow (CBF), abnormal oxygen extraction fraction (OEF), and ultimately lead to oxygen deprivation of the brain tissue (Adams et al. 2007., Cheung et al. 2002), however, the underlying pathophysiology is not well understood. While much research has focused on the role of vasculopathy in neurologic injury in SCD, over one third of children with sickle cell disease who suffer an overt ischemic event do not present with arterial stenosis (Hulbert et al. 2011). Extending the work of Nur et al. (2009), we have recently shown in children without stenosis in SCD that elevated cerebral blood flow and diminished cerebrovascular reserve is associated with the severity of anemia (Kosinski et al. 2015). However, to date, little is known about the relative contributions of non-vasculopathic hemodynamic compromise that may occur in children with SCD. Therefore, a comprehensive model of pathophysiology in this population will help stratify stroke risk and guide therapeutic strategies.
Aim:
To noninvasively quantify both CBF and OEF in children with SCD using magnetic resonance imaging.
Methods:
11 patients (7M/4F; age 14 ± 2.7 years (mean ± SD)) with SCD and no history of stroke nor arterial stenosis were imaged on a 3T MRI system. 9 patients were on hydroxyurea (average dose: 19.7 ± 3 mg/kg/day). Hematological parameters were acquired at a clinic visit no more than one month prior to the MRI scan (Table 1). Pulsed arterial spin labelling MRI was used to noninvasively assess grey matter cerebral blood flow according to a standard kinetic model. A T2*-weighted flow-compensated image provided phase information, with the phase signal difference between the sagittal sinus and surrounding tissue used to quantify venous oxygenation (SvO2) (Driver et al. 2014). Arterial oxygen saturation (SaO2) was measured via peripheral pulse oximetry and OEF was determined by (SaO2 - SvO2/SaO2) according to Fick's principle of arteriovenous difference.
Results:
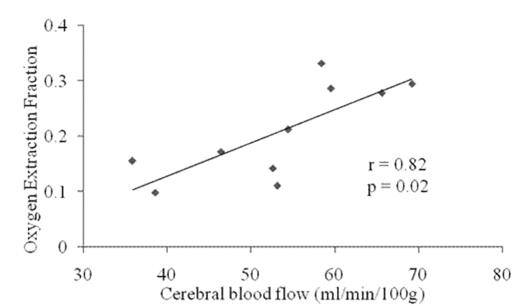
A significant positive association was observed between CBF and OEF (p = 0.82, p = 0.02, pearson product moment correlation coefficient), as shown in Figure 1. Mean values (± SD) were 0.75 ± 0.08, 0.23 ± 0.08 and 54.1 ± 11 ml/min/100g for SvO2, OEF and CBF respectively.
Discussion:
The observed correlation between CBF and OEF suggests that children with SCD who do not present with vasculopathy, utilize both the perfusion and metabolic reserve in order to meet the cerebral demand for O2. This allows CBF and OEF to increase simultaneously rather than sequentially as proposed by Powers et al. (1991). This non-sequential hemodynamic compromise is in agreement with previous literature in cerebrovascular disease (Kanno et al. 1988) and may serve to minimise increases in cardiac output (Varat et al. 1972). This data suggests that elevated OEF may serve as an early risk marker for overt stroke in addition to elevated blood flow velocity and thus may help better screen for those who will most benefit from transfusion therapy.
| . | SCD Patients . | . | . |
|---|---|---|---|
| Sample Size (N) | 11 | ||
| Gender (M/F) | 7/4 | ||
| Age (y) | 13.7 ± 2.7 | ||
| BMI (Kg/m2) | 18.8 ± 3.0 | ||
| Hematocrit | 0.282 ± 0.03 | ||
| Hemoglobin (g/L) | 100 ± 10.3 | ||
| SaO2 | 0.99 ± 0.02 | ||
| SvO2 | 0.75 ± 0.08 | ||
| Absolute Reticulocyte (K/uL) | 205 ± 72 | ||
| Neutrophil Count (K/uL) | 5.3 ± 3.7 |
| . | SCD Patients . | . | . |
|---|---|---|---|
| Sample Size (N) | 11 | ||
| Gender (M/F) | 7/4 | ||
| Age (y) | 13.7 ± 2.7 | ||
| BMI (Kg/m2) | 18.8 ± 3.0 | ||
| Hematocrit | 0.282 ± 0.03 | ||
| Hemoglobin (g/L) | 100 ± 10.3 | ||
| SaO2 | 0.99 ± 0.02 | ||
| SvO2 | 0.75 ± 0.08 | ||
| Absolute Reticulocyte (K/uL) | 205 ± 72 | ||
| Neutrophil Count (K/uL) | 5.3 ± 3.7 |
Clinical parameters acquired within 30 days of the MRI session
A significant positive association was observed between grey matter cerebral blood flow and oxygen extraction fraction (r = 0.76, p = 0.002) in children with sickle cell disease
A significant positive association was observed between grey matter cerebral blood flow and oxygen extraction fraction (r = 0.76, p = 0.002) in children with sickle cell disease
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.