Abstract
Introduction
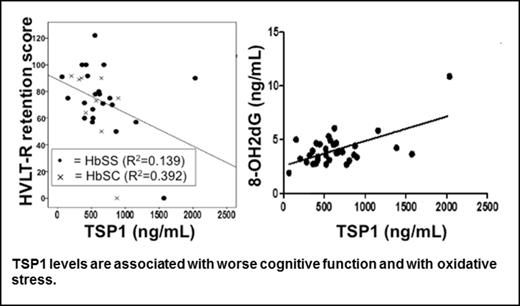
Cognitive impairment (CI) is a serious complication of sickle cell disease (SCD) with a prevalence of more than 40% (Vichinsky, JAMA 2010). It is responsible for functional limitations in schooling in children and in occupation and compliance with therapy in adults, and is therefore recognized as both a medical and social devastation of SCD. While the pathophysiology of SCD-related cognitive impairment is not fully elucidated, SCD patients are exposed to high levels of chronic inflammation and oxidative stress, which are responsible for cognitive impairment in other vascular diseases, suggesting that these factors may also play a role in SCD. Thrombospondin-1 (TSP1) is a secreted protein that stands at the crossroads of multiple inflammatory and oxidative pathways crucial to the SCD pathology (Isenberg, PNAS 2005, JBC 2006, Blood 2008, Csanyi, ATVB 2012; Yao, JASN 2014). Importantly, TSP1 levels are elevated in patients with SCD and correlate with an increased risk of vaso-occlusive complications in adults (Novelli, AJH 2012) and a higher burden of silent cerebral infarcts in children (Faulcon, BJH 2013). Herein, we explored the association between TSP1, oxidative stress and cognitive function in a cohort of patients with SCD.
Methods
Thirty-four SCD patients (HbSS, HbSC and HbS/β-thalassemia) >18 years and in steady state were recruited from the UPMC Adult Sickle Cell Program outpatient clinic (Pittsburgh, PA). Upon obtaining informed consent, patients underwent a blood draw and the Hopkins Verbal Learning Test - Revised (HVLT-R), a test of episodic memory whose scores are associated with cerebral small vessel disease in SCD patients (Novelli, PRN 2015). Platelet-poor plasma was collected and stored for analysis by ELISA of TSP1 and the oxidized derivative of deoxyguanosine, 8-hydroxy-2-deoxy guanosine (8-OH2dG), a marker of oxidative stress. Statistical analyses were completed using SAS 9.3.
Results
SCD patients had a mean age of 35 (22-65), were 65% female, 66% had greater than high school education, and 65% had HbSS disease, 30% had HbSC disease, and 5% had S/β-thalassemia. Elevated plasma TSP1 levels correlated inversely with HVLT-R retention score (standardized b=-0.457, p=0.007). Conversely, elevated plasma TSP1 levels positively correlated with increased levels of plasma 8-OH2dG (standardized b=0.361, p<0.001). The association between TSP1 and HVLT-R was potentiated after adjustment for 8-OH2dG (standardized b=-0.762, p<0.001). Moreover, the association between 8-OH2dG and cognitive function was also significant after adjusting for TSP1 (standardized b=-0.633, p=0.015).
Discussion
Elevated plasma TSP1 levels are associated with poorer episodic memory in SCD patients. This is the first evidence of a link between a plasma protein associated with vascular disease and cognitive function in adults with SCD. TSP1 levels were also positively correlated with 8-OH2dG, and adding 8-OH2dG to the model of TSP1 and HVTL-R retention appeared to increase the detrimental effect of TSP1. These results suggest that the effect of 8-OH2dG on cognitive function becomes evident only in the presence of higher TSP1 levels and implicate oxidative stress as intermediary to the effect of TSP1 on cognitive function in SCD.
Isenberg:RCTI, Inc.: Equity Ownership, Patents & Royalties: US Patent No. 8236313; Vasculox, Inc.: Equity Ownership, Patents & Royalties: US Patent No. 8236313.
Author notes
Asterisk with author names denotes non-ASH members.