Abstract
Introduction: The prognosis of patients with a FLT3-ITD mutation in acute myeloid leukemia (AML) is worse than FLT3 wild type patients, with increased early relapse including after allogeneic stem cell transplantation (SCT) and with a poor response to salvage. FLT3-ITD mutant patients who relapse after SCT or fail salvage chemotherapy have a dismal prognosis with no approved treatment options. Quizartinib (AC220), an oral FLT3 receptor tyrosine kinase inhibitor, has shown a remission rate of 44%, and median overall survival of 23 weeks in FLT3-ITD mutant patients who were relapsed or refractory to 2nd line treatment, or relapsed following SCT in a non-randomised phase 2 study [1]. While these outcomes compare favourably to published data, which give a median survival of 1.5 months in all comers [2], and median survival in FLT3-ITD mutant patients of 13 weeks following first relapse [3], there is an overall paucity of data available for the FLT3-ITD+ subpopulation examined in the quizartinib studies . The UK NCRI database is the largest dataset for FLT3-ITD+ AML patients, containing 6872 patients with ITD status (1388 mutant) and systematic collection of data from diagnosis with follow-up for at least 5 years or to death.
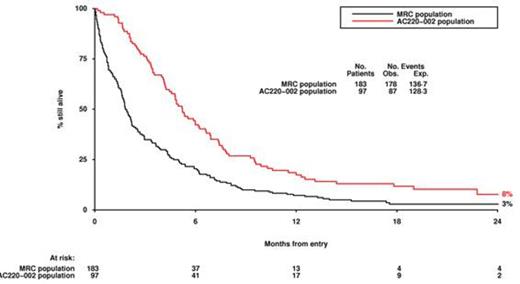
Methods: 97 FLT3-ITD+ patients from the AC220-002 study who had received intensive chemotherapy, and had either relapsed following SCT (n=39); or were relapsed (n=53) or refractory (n=5) following salvage therapy prior to enrolment were identified. The equivalent eligibility criteria were applied to the UK MRC/NCRI database of AML trial patients treated intensively from 1988-2013 who had confirmed FLT3-ITD mutation: 183 patients matching the same criteria were identified (post-SCT n= 65; relapsed n=99; refractory n=19). Patients in this group received only recognised intensive chemotherapy regimens prior to fulfilling the eligibility criteria. To reflect the screening period in AC220-002, patients in the MRC/NCRI cohort entered the analysis 14 days following being identified as relapsed/refractory. The primary endpoint was overall survival. Multivariable Cox/logistic regression was performed stratified for known prognostic factors, including route to eligibility (post SCT/relapsed/refractory). Sensitivity analyses were performed excluding deaths within 14 and 28 days from eligibility from the MRC/NCRI cohort only to allow for patients who might not have been considered for quizartinib treatment on grounds of fitness.
Results: There was no significant difference in the ages of the two cohorts (median age AC220-002 47y vs. MRC 48y). Outcomes in the MRC/NCRI cohort did not improve over time from 1988-2013 (p=0.7). Analyses were performed adjusted for route to eligibility, ITD allelic ratio, duration of remission (in relapsed patients), and cytogenetics. Overall survival was improved in the Quizartinib patients (adjusted hazard ratio (HR) 0.40 (0.29-0.55) p<.0001), with no interaction with route to eligibility (p=0.4). Median survival was 231 vs 60 d for relapse post SCT, 128 vs 53 d in relapsed patients, and 146 vs 61 d in refractory patients. Response rates (CRc) overall were 43% vs 11% (adjusted OR 0.24 (0.10-0.61) p=0.002). In sensitivity analyses excluding deaths within 14 days (HR 0.50 (0.36-0.69), p<.0001) and 28 days (HR 0.5 (0.38-0.76) p=0.0004) within the MRC/NCRI cohorts quizartinib retained superiority.
Discussion: Quizartinib has previously shown activity in relapsed/refractory patients in a large Phase 2 single arm study, and is currently being studied in a randomized Phase 3 study vs. standard salvage chemotherapy. This analysis examines a patient population that has failed salvage therapy or SCT and for whom there is no standard therapy. It confirms the prolonged overall survival seen in the Phase 2 study when compared to an equivalent large historical cohort of previously intensively treated patients from the UK MRC/NCRI trials, with median survival in quizartinib patients was 159 days compared to 56 days in the historical cohort. Even if deaths within 28 days are excluded entirely from the MRC/NCRI group, there is a highly significant survival benefit for quizartinib. Overall, the activity seen in the AC220-002 Phase 2 study is greater than that seen in comparable patients in a large historical cohort.
[1] Levis M et al. ASH meeting Abstr 615, 2014. [2] Giles F et al. Cancer 104 (3), p547, 2005. [3] Ravandi F et al. Leukemia Research 34, p752, 2010.
Off Label Use: Quizartinib for AML. Gammon:Ambit: Employment. Trone:Ambit: Employment.
Author notes
Asterisk with author names denotes non-ASH members.