Abstract
Background:
Deletions in the Ikaros gene (IKZF1) have been associated with a poor outcome in pediatric B-ALL, but the interaction of IKZF1 deletions with other established prognostic factors, such as minimal residual disease (MRD), is still under investigation. Here we report the IKZF1 deletion status of 405 patients (pts) with acute lymphoblastic leukemia (ALL) and its association with other presenting features, end-induction MRD, and outcome.
Methods:
Between 2005-2011, 794 eligible pts (aged 1-18 yrs) with newly diagnosed pediatric ALL (B-ALL: 697; T-ALL: 97) were enrolled on DFCI ALL Consortium Protocol 05-001. End-induction MRD was assessed prospectively on all pts by allele-specific oligonucleotide-PCR assay. DNA was extracted from archived diagnostic blood or bone marrow samples from 399 B-ALL and 6 T-ALL pts with sufficient available material. Using a commercially available kit (SALSA MLPA P202 IKZF1, MRC-Holland), IKZF1 deletion status was assessed by multiplex ligation-dependent probe amplification (MLPA). Event free survival (EFS) and relapse free survival (RFS) were estimated using the method of Kaplan and Meier.
Results:
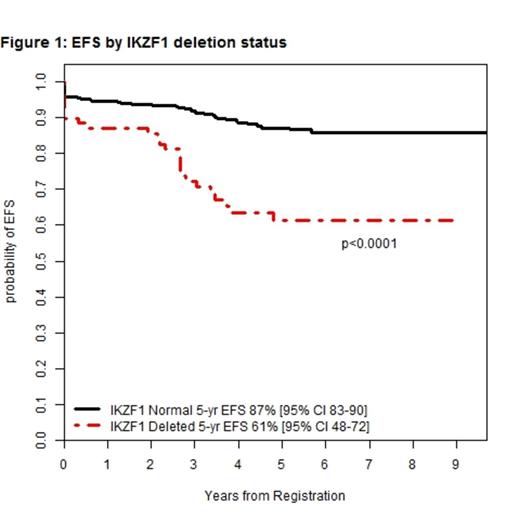
IKZF1 deletion was detected in 69 (17%) of the 405 evaluated pts. IKZF1 deletion was more common in pts over 10 years old (p<0.0001), males (p=0.05), Hispanic/Latinos (p=0.002) and those with presenting white blood cell count (WBC) at diagnosis ≥ 50K/ul (p<0.0001). IKZF1 deletions were detected in 7 of 13 (54%) pts with the Philadelphia chromosome (Ph+). Significantly more IKZF1 pts experienced induction failure (7% vs 1%, p=0.009) and relapse (25% vs 7%, p<0.0001) than pts without IKZF1 deletions. There was no difference in rates of treatment-related mortality. With a median follow-up of 5.3 years, the 5-year event free survival (EFS) for patients without IKZF1 deletion was 87% and 61% for those with IKZF1 deletion (p<0.0001; Figure 1). There was no significant difference in EFS based on type of IKZF1 deletion: 1) deletions of exons 4-7 or 4-8 (42% of cases, 5-yr EFS 51%) or 2) whole gene (49% of cases, 5-yr EFS 69%) (p=0.23).
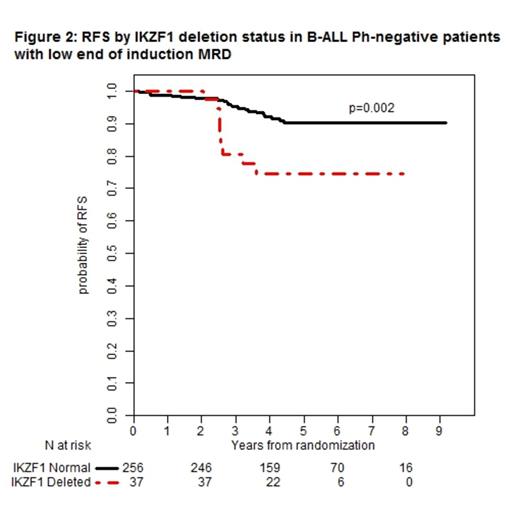
315 Ph-negative B-ALL pts achieving complete remission (CR) had assessable end-induction MRD. Significantly more IKZF1 non-deleted pts had low MRD compared with IKZF1-deleted pts (95% vs 82%, p=0.006). For the 293 MRD-low pts, relapse occurred in 7% of IKZF1 non-deleted and 24% of IKZF1-deleted pts (p=0.004); for 22 MRD-high pts (all of whom received intensified therapy), there was no significant difference in relapse between IKZF1 non-deleted and IKZF1-deleted pts (21% vs 37%, p=0.62). The 5-yr relapse-free survival (RFS) was significantly worse for MRD-low pts with IKZF1 deletions versus those without these deletions (Figure 1). In multivariable analysis, IKZF1 status, but not MRD, was significantly associated with RFS for Ph-negative B-ALL pts. (Table 1)
Conclusions:
IKZF1 deletion is associated with higher rates of induction failure and relapse, and is a significant predictor of inferior outcome in pediatric B-ALL. IKZF1 deletion was associated with significantly higher rates of relapse in Ph-negative B-ALL patients with low end-induction MRD, and thus may be useful factor to consider when stratifying treatment intensity in this subset of pts. We conclude that IKZF1 deletion should be incorporated into risk stratification for pediatric B-ALL.
Prognostic Factors for RFS for B-ALL, Ph-negative pts with evaluable end-induction MRD
| . | Univariate . | Multivariable . | ||
|---|---|---|---|---|
| HR [95% CI] . | p-value . | HR [95% CI] . | p-value . | |
| Age, ≥10 vs <10 | 1.40 [0.68-2.91] | 0.36 | 1.19 [0.56-2.51] | 0.65 |
| IKZF1, del vs. not | 3.23 [1.61-6.45] | 0.0009 | 2.53 [1.20-5.30] | 0.01 |
| MRD, high vs. low | 2.51 [1.04-6.03] | 0.04 | 1.63 [0.64-4.11] | 0.30 |
| WBC, ≥50 vs. <50 | 2.50 [1.27-4.94] | 0.008 | 1.99 [0.98-4.03] | 0.06 |
| . | Univariate . | Multivariable . | ||
|---|---|---|---|---|
| HR [95% CI] . | p-value . | HR [95% CI] . | p-value . | |
| Age, ≥10 vs <10 | 1.40 [0.68-2.91] | 0.36 | 1.19 [0.56-2.51] | 0.65 |
| IKZF1, del vs. not | 3.23 [1.61-6.45] | 0.0009 | 2.53 [1.20-5.30] | 0.01 |
| MRD, high vs. low | 2.51 [1.04-6.03] | 0.04 | 1.63 [0.64-4.11] | 0.30 |
| WBC, ≥50 vs. <50 | 2.50 [1.27-4.94] | 0.008 | 1.99 [0.98-4.03] | 0.06 |
[HR=Hazard ratio]
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.